The Neuromuscular Rebalancing of the Stomatognathic System: The Feedback System
Dr. Piero Silvestrini Biavati
Neuromuscular Rebalancing of the Stomatognathic Apparatus: Feedback System
Dr. Piero Silvestrini Biavati, Private Practitioner in Genoa, Specialist in Odontostomatology, PhD
Dr. Franco Guida, Private Practitioner in Genoa, Specialist in Odontostomatology
INTRODUCTION
The issue of craniofacial muscle relaxation has been addressed multiple times by various authors in recent years. The importance of this technique in diagnosing and treating pain-dysfunction disorders is immense. Without relaxation, we cannot determine what kind of rehabilitation to plan, mainly for two reasons:
a) the patient is symptomatic and we cannot predict the benefits of our intervention (1).
b) the patient is symptomatic and therefore their mandibular-cranial relationship is not only altered but also beyond their adaptive range, enough to trigger pain (2).
Several relaxation aids have been proposed, from cotton rolls (3) to anterior jigs (4), to various types of upper, lower, partial, rigid, and flexible splints (5), electromyographic biofeedback (6,7), up to the use of T.E.N.S. (8). All these systems can work, but they all present intrinsic difficulties that limit their use in our clinics (9-11).
PHYSIOLOGY OF OCCLUSION
Before briefly reviewing these systems, it is important to clarify how and why the neuromuscular system contracts. Occlusal proprioception occurs during swallowing, or at least whenever the dental arches contact each other (12). This allows our brain to always know where to move the mandible to bite, chew, or simply swallow. But to do this, it is vital, for the protection of our dental pillars and joints, to continuously "refresh" the current situation in memory. Why continuous? It's simple: consider the act of chewing. Food is progressively crushed based on its size and resistance, with increasing force until dental contact is made, triggering the swallowing reflex. Our neuromuscular system "tests" the food's consistency each time it is bitten, acquiring knowledge of what it is facing. For example, biting a sandwich: it is bitten gently, and progressively the necessary force is applied to cut it. The applied force depends on its consistency; a toast is bitten with less force than a day-old sandwich, but the start of the action is the same. Another example is chewing a piece of meat, where the force used is high after some chewing cycles. But if you accidentally bite down on a lead pellet in the food, you risk breaking a tooth because the system did not expect such resistance. If the pellet is sensed briefly between teeth, chewing becomes gentle and cautious, never reaching maximum intercuspation, until the foreign object is identified and removed. Moreover, the pellet can remain between teeth safely, as its presence and size are memorized from even a fleeting contact. Hence the refresh must be continuous (13). Once we clarify how the system controls occlusion, we see how it can enter pathological contraction. For example, after a new filling, the patient may report it feels slightly high; the dental arches contact only at the filling point. We know that at least three points of contact are necessary for stability. The system cannot remain in an unstable equilibrium; it needs to "rest" evenly, like standing on toes briefly before settling fully on the sole. The mandible moves imperceptibly with each swallow to find these three points. This movement is mainly performed by the muscles responsible for mandibular spatial positioning: the Temporalis and Internal and External Pterygoids. Then the filling no longer feels high. This continuous adaptation allows us to function despite small issues without "breaking" like machines. We compensate wear, tooth fractures, bridges, fillings, malocclusions, but constant compensation can lead to significant deviations causing severe pain syndromes. For example, kyphoscoliosis can cause "hunchback" with all its functional and painful limitations. Within our field, cervical pathologies, headaches, joint disorders, and postural alterations can develop.
CLINICAL APPLICATIONS
Thus, all types of jigs and splints can temporarily "reset" the system, promoting new programming for stable occlusion. If the splint is well-positioned, all goes well; otherwise, a new adaptation begins. Patients often report symptom improvement but may relapse after days. It is challenging to create a splint without interference and even harder to calculate a correct mandibular-cranial relationship under neuromuscular equilibrium when the system is highly contracted (14).
Since 1969 (15-19), a novel idea developed: a hydrostatic splint based on communicating vessels (Photo 4)—two soft fluid-filled sacs connected to allow free fluid flow. Dysfunctional patients find two soft cushions between their arches when swallowing, freeing them from dental interference.

The greater pressure on one side pushes fluid to the opposite side, triggering a feedback mechanism (Photo 3) normalizing involved muscles within minutes. These cushions provide essential support for neuromuscular normalization. The patient, using reflexive functions involuntarily, gradually reaches equilibrium. These splints were complex to make but are now available as preformed pseudoplates in three sizes fitting most dental arches, provided sufficient teeth remain (Photos 1 and 2).


MATERIALS AND METHODS
To verify efficacy, 60 patients were monitored and tested habitually (WAQ, Without Aqualizer®), minutes after Aqualizer® application (AQ), and after 12 hours (AQ12) across 31 parameters. Patients were self-referred with no pre-selection, all dysfunctional seeking pain relief.
Equipment: 4-channel Myotronics EMG, Myotronics K6I Diagnostic Kinesiograph (Photo 5), Scoliosometer with weight indication (20).
Tests conducted:
EMG of Temporalis and Masseters at rest (TRP/MRP) to assess electrical activity asymmetry Dx/Sin (%).
EMG of Temporalis and Masseters during clench (TCL/MCL) for electrical activity asymmetry Dx/Sin (%).
Kinesiography and EMG to analyze swallowing patterns: Infantile (VS), Atypical (AS), Correct (SS) (21).
Kinesiography (Scan 1) for movement disorders like dyskinesia (OCV), frontal crossover (FC), sagittal crossover (SC), meniscal incoordination (ID), mouth opening side shift (MOSS).
Objective exam of frenulum median alignment (FMA), max mouth opening (MMO).
Intraauricular palpation for condylar retrusion (LCR/RCR).
Palpation of joint clicks in first third of movement (ROC/LOC/RCC/LCC).
Palpation of tenseness in internal and external pterygoid muscles (IPD/EPD) rated 0-3.
Differential diagnosis of muscular, articular, mixed pain (AP/MP/AMP).
Evaluation of muscle headaches (MH) and cranio-cervical pain (CP).
Kinesiological tests of psoas (AK) with resistance 1-3.
Apparent leg length (LL).
Scoliosometer weight distribution (WDS).
Head rotation limitation (HR) 0-3.
RESULTS
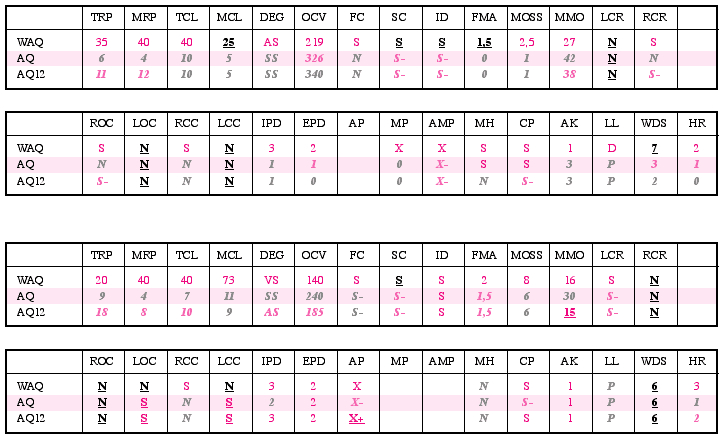
Below is a typical table for patients with myogenous or mixed pathology (37 total), showing average values.
Legend:
AP - Arthrogenous Pain
AMP - Arthrogenous and Myogenous Pain
AQ - Aqualizer®
AQ12 - Aqualizer® for 12 hours
AK - Applied Kinesiology
AS - Atypical Swallow
CP - Cervical Pain
DEG - Deglutition
EPD - External Pterygoid Digital palpation
FC - Frontal Crossover
FMA - Frenulum Medialis Alignment
HR - Head Rotation
ID - Internal Derangement
IPD - Internal Pterygoid Digital palpation
LCC - Left Closing Click
LCR - Left Condylar Retrusion
LL - Legs Length
LOC - Left Opening Click
MCL - Masseters Clench
MH - Muscular Headache
MMO - Max Mouth Opening
MOSS - Mouth Opening Side Shift
MP - Myogenous Pain
MRP - Masseters Rest Position
OCV - Open-Close Velocity
RCC - Right Closing Click
RCR - Right Condylar Retrusion
ROC - Right Opening Click
SC - Sagittal Crossover
SS - Somatic Swallow
TCL - Temporalis Clench
TRP - Temporalis Rest Position
VS - Visceral Swallow
WAQ - Without Aqualizer® (habitual)
WDS - Weight Distribution Scoliometer
CONCLUSIONS
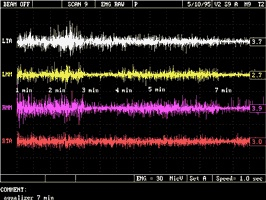
Fig. 6 Typical relaxation of Temporalis and Masseters over time starting from habitual condition with Aqualizer® insertion.
A 2-second EMG reading was taken every minute.
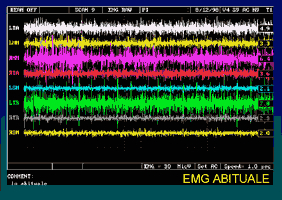
Fig. 7 EMG status with different relaxation types: habitual.
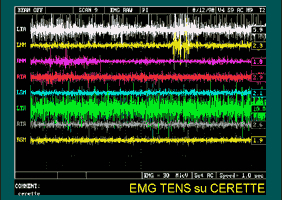
Fig. 8 EMG status with various relaxations: 45 minutes TENS on Kerr Occlusal Indicator Wax.
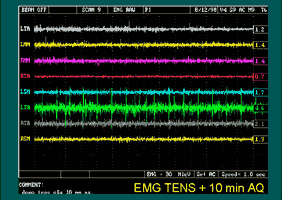
Fig. 9 EMG status with various relaxations: after 45 minutes TENS is turned off and 10 minutes Aqualizer® is applied.
NB - Color differences in the graphs (figs. 6-7-8-9) only highlight histogram excursions.
In myopathy and myoarthropathy cases, results were remarkable: temporalis and masseter rebalancing occurred in about 8 minutes, with nearly perfect muscular symmetry (Photo 6), much better than achievable with T.E.N.S., previously our best. Pterygoids were less painful on palpation within about 20 minutes, somewhat matching prior jig research (28), though jigs seem more effective. EMG clench tests always showed simultaneous contraction of all four muscles, similar to cotton roll tests, indicating potential balanced support (29). Resting EMG varied with relaxation type: photo 7 shows habitual strong asymmetries; photo 8 highlights 45 min TENS effects with mixed relaxation, causing more imbalance. Using Aqualizer‘ for 10 min (photo 9) resulted in more homogeneous, balanced relaxation. Kinesiographic and EMG swallowing analysis showed most patients with atypical or infantile swallowing immediately normalized to type 1 swallow, possibly reducing need for corrective myofunctional swallowing exercises in pathology (30).
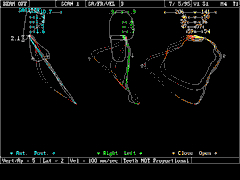
Fig. 10 Typical change with Aqualizer®: reduction in meniscal incoordination and consequent less frontal deviation.
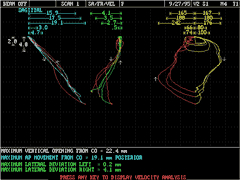
Fig. 11 Habitual: opening and closing trajectory and speed.
Kinesiography Scan 1 indicates improved open-close velocity, reduced meniscal incoordination, better frontal trajectories with less deviation (Photos 10 and 11).

Fig. 12 Scoliosometer variation induced by Aqualizer®: weight realigns, head rises, and rotation improves.

Fig. 13 Habitual: opening and closing trajectory and speed.

Fig. 14 Same patient: postural dysfunction.
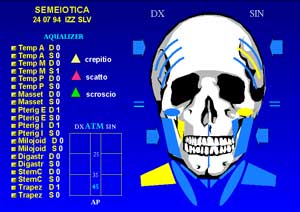
Fig. 15 Same patient: head and neck dysfunction after 20 min. with Aqualizer®.

Fig. 16 Same patient: postural dysfunction after 20 min. with Aqualizer®.
Photos 13-16 show the pain-dysfunction changes after just 20 minutes: less muscle soreness, increased max mouth opening, reduced clicks and condylar retrusion, midline realignment, and activation of elevator muscles during clenching. Kinesiological tests were positive, with improved muscle resistance and tendency toward leg alignment (31).

Photo 12, on the Scoliosometer, shows significant postural changes. On the left, the patient in habitual condition has body shifted left with a 6 Kg weight imbalance, but also is taller, stands more upright, has changed shoulder posture (32), arms appear longer, can rotate head more, able to see vertical red lines behind more centered (20). Note the patient did not move on the platform; changes were induced quickly by repeated swallowing. All parameters improved, mostly in first 20 minutes; after 12 hours improvement was often less significant. Patient wore Aqualizer‘ all night and came to clinic without removing it; instructed to perform oral hygiene only with mouthwash and have a liquid breakfast to avoid returning to habitual occlusion and proprioceptive reconditioning. The "surprise" effect of this device could cause false improvement, but more likely the bite’s elastic effect causes continuous chewing exercise that limits muscle relaxation and reduces interocclusal thickness and vertical dimension. This might reduce benefits for related conditions like neck pain, max mouth opening, or opening/closing speed. This suggests the device is not suitable for long-term therapy. However, used diagnostically on occlusion influence on pathology (e.g., headaches, vertigo), results were exceptional, sometimes creating near dependency syndrome due to benefits. Important was ability to immediately check for disappearance of clicks and joint noises (33). Using anterior jig transferred Aqualizer‘ neuromuscular position to models for making diagnostic-rehabilitative splints, orthotics, and night splints, bite planes, and night guards for bruxism with better results than manual manipulation, reducing adjustments needed.
In cases of advanced arthropathy, results were mixed. At 12 hours, improvements were often less, probably for above reasons. Notably, some parameters systematically worsened: arthrogenous pain, max mouth opening, and clicks. For first two, chewing activation or stabilization control systems via clenching or tongue likely cause small mandibular movements raising pain and muscle contraction. Click increase probably false worsening as locking joints with stretched meniscal ligament start partial disc recapture producing clicks (13). Tests avoided meniscus recapture to not falsify results. This suggests Aqualizer‘ alone cannot fully recapture displaced discs, but after 20 minutes disc recapture is easier and less painful, confirming muscle relaxing effect.
Numbers in purple indicate pathology, light blue italic improvement, bold purple underline worsening, light purple italic minor improvement.




