Correlation Between Postural Alterations and Dental Occlusion Problems
Dr. Daniela Costa
University of Genoa
School of Medical and Pharmaceutical Sciences

Degree Course in Physiotherapy
Coordinator: Prof. C. Gandolfo
Correlation between postural alterations and dental occlusion problems: evaluation of the scope of competence and the role of the physiotherapist in the multidisciplinary corrective-rehabilitative treatment.
Supervisor: Prof. Marco Mezzasalma
Candidate: Daniela CandidatoCosta
Academic year 2011-2012
CHAPTER 1
STOMATOGNATHIC SYSTEM
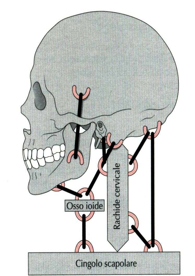
The stomatognathic system is an anatomical-functional complex composed of organs and tissues that perform digestive functions (salivation, chewing, swallowing), respiratory and relational functions (phonation, facial expression). This system consists not only of the mandible and TMJ, but also the cervical spine, the hyoid bone, the pharyngeal complex, teeth, tongue, vascular and lymphatic systems, and finally the neuromuscular system that interacts with these structures.
TEMPORO-MANDIBULAR JOINT
1.1 Articular Anatomy
The Temporo-Mandibular Joint (TMJ) is a double condyloid diarthrosis established between the two mandibular condyles and the mandibular fossae of the two temporal bones. By definition, it is mobile and provided with a synovial membrane. The joint is considered double because between the mandibular condyle and the articular cavity of the temporal bone there is a fibrocartilaginous disc (the meniscus) that divides the articular cavity into two non-communicating parts; thus, the joint is divided into two sectors: temporo-meniscal and mandibulo-meniscal or condylo-meniscal. The articular surface of the mandible is constituted by the mandibular condyle which, at the summit of the condylar process, forms an ellipsoidal projection with the major axis directed medially and backward. The temporal articular surface is given by the anterior part of the mandibular fossa and the articular tubercle of the zygomatic process. The mandibular articular surface can be more specifically divided into three zones called postero-anteriorly: fossa proper, eminence, and temporal crest
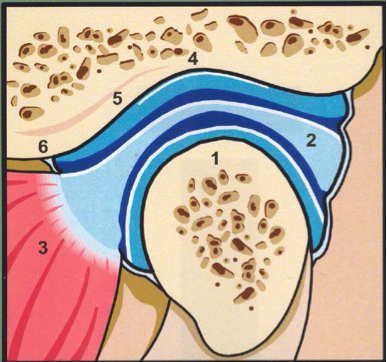
1: MANDIBULAR CONDYLE. 2 ARTICULAR MENISCUS. 3 INFRATEMPORAL HEAD OF EXTERNAL PTERYGOID MUSCLE. 4 TEMPORAL FOSSA. 5 TEMPORAL EMINENCE. 6 TEMPORAL CREST
The two opposing articular surfaces are incongruent. Congruence is established by the presence of the articular meniscus, which is biconcave in shape and maintained antero-posteriorly by its morphology and concavities that articulate with the convexities of the condyle and the articular eminence, and medio-laterally by the collateral ligaments (which connect it to the medial and lateral poles of the mandibular condyle).
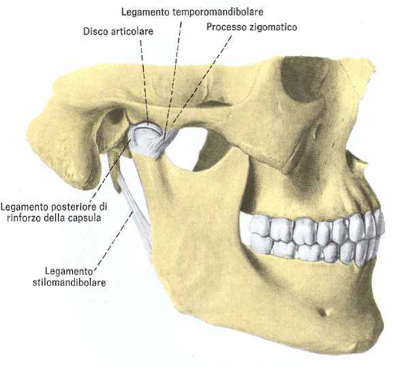
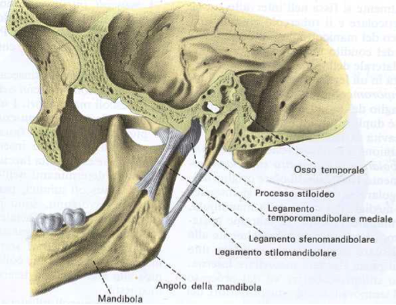
The joint connection means are given by the articular capsule and the distant ligaments. The former surrounds the entire joint and is reinforced by the posterior reinforcing ligament and anteriorly by the temporomandibular ligament; among the latter, we distinguish the sphenomandibular ligament and the stylomandibular ligament, which originate respectively from the angular spine of the sphenoid and the temporal styloid process and then insert on the
medial surface and posterior margin of the mandibular ramus. Among the extrinsic ligaments of the joint, the pterygomandibular ligament can be counted, an aponeurotic structure that extends from the hook of the medial wing of the pterygoid process of the sphenoid to the posterior end of the internal surface of the alveolar process of the mandible.
1.2 Articular Physiology
The human temporomandibular joints (TMJs) combine the dynamic-morpho-functional characteristics of carnivorous and
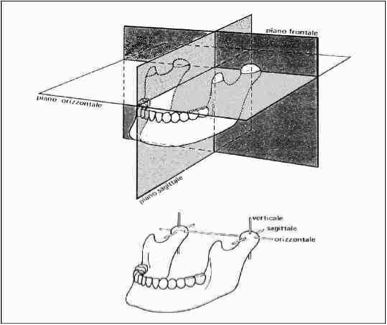
herbivorous species. Carnivorous animals have a hinge joint suited to opening and closing movements, i.e., vertical force actions only. In herbivores, lateral movements are mainly developed. The TMJs of primates, and particularly humans, have a morphology resulting from the effects of right-left laterality as well as circumduction movement, which is the sum of all others. All these movements are possible thanks to a group of muscles belonging to the skull and neck (masticatory muscles). During any mandibular movement, the joints on both sides act simultaneously and in coordination; therefore, the movement of the mandible must be studied considering both joint points. Movements occur through combined rotation and translation of the condyles in three planes of space: median sagittal, frontal, and horizontal. To describe mandibular movements in space, we must identify the reference planes and the axes around which the condyles rotate. The three planes mentioned are orthogonal: the median sagittal plane is vertical and passes through the interparietal suture dividing the skull into two mirror halves, right and left; the frontal plane separates front and back; the horizontal plane separates the upper from the lower part. Regarding condylar rotation axes, rotation can occur around three axes: horizontal, vertical, and antero-posterior; only the horizontal axis is common to both condyles (called the bicondylar axis). This divides the skull into anterior and posterior parts. The vertical and antero-posterior axes are monocondylar, each condyle having its own axis. When the condyles rotate around the bicondylar axis, their rotation is always consensual and the mandible moves in the sagittal plane. Rotation around the other two axes involves rotation of only one condyle at a time (rotating condyle) while the other (contralateral) performs a translatory or orbiting movement describing an arc (orbiting condyle). The elementary mandibular movements are three types:
· Opening and closing movement
· Protrusion and retrusion movements
· Lateral translation movements
OPENING AND CLOSING MOTION
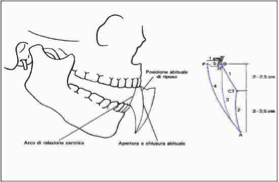
These are movements performed in the sagittal plane, carried out with rotation of the condyles around the bicondylar axis or combined translation and rotation of the condyles. The lowering movement can start from centric occlusion or from the mandibular rest position. In the first case, the occlusal surfaces of the antagonistic dental arches have maximum contact (intercuspidation), while in the second case there is a small space between the occlusal surfaces of the opposing arches and the mandible has a slight degree of opening. The transition from centric occlusion to rest position occurs through a rotation of about 2 degrees of the condyle head around the bicondylar axis, using the condyle-disc joint. Considering the opening movement from either position, mandibular movement can be divided into two phases: rotation and translation of the condyles. Rotation around the bicondylar axis is about 10-12 degrees counterclockwise, creating a distance of 2-2.5 cm between the upper and lower incisor margins. During rotation, the translatory motion of the condyles is 1-2 mm, but the mandible lowers further due to bilateral translation of the condyles, which simultaneously move downward and forward along the condylar path. In this position, the condyle head can perform an additional rotation that shifts it up to the apex of the articular tubercle, so that at maximum opening the space between the upper and lower incisors is 5-6 mm. During mandibular closing motion, which presumably begins at maximum opening, there is a simple rotation of the condyle in the opposite direction, followed by combined rotation and translation as it returns into the temporal cavity.
PROTRUSION AND RETRUSION MOVEMENTS IN THE HORIZONTAL PLANE
These movements occur in the horizontal plane with the lower dental arch sliding over the upper one, carried out by translation of the condyles, with minimal rotation. The condylar movements are bilateral and simultaneous. The range of forward projection movement is the same as in maximum mandibular opening; in the case of maximum sliding, the lower incisors protrude beyond the upper by 7-10 mm. Retraction is the reverse movement.
LATERALITY MOVEMENTS IN THE HORIZONTAL PLANE
These movements occur in the horizontal plane and allow the mandible to translate right and left. Lateral movements occur with the mandible both closed and open; in the first case with sliding of the occlusal surfaces of opposing teeth, in the second when the condyles have mobility in the articular cavities. In other phases, lateral movements are minimal. These lateral movements are performed as follows: one condyle rotates around the vertical axis (rotating condyle), while the other (contralateral) undergoes a translatory movement describing a small arc (orbiting condyle). When the mandible moves to the right, movement occurs by rotation of the right condyle, which acts as a pivot, around the vertical axis. The rotating condyle always undergoes slight rotation with lateral and posterior displacement, while the orbiting condyle is shifted forward. The lateral movement of the mandible is also called abduction, the return to rest position is called adduction.
MANDIBULAR MOTION IN THE SAGITTAL PLANE
To describe this movement, a point
located in the central interincisal space of the mandible starting from the condyle position in centric occlusion, and following this point during mandibular opening and closing movements, can be observed to perform on the sagittal plane a
diagram described in Figure 6 (Posselt’s diagram). The scheme can be described as follows: starting from the centric occlusion position (O) or the rest position (R), then the mandible lowers describing a centric relation arc (1) until the terminal point CT, from here opening continues by translation of the condyles (2). Upon reaching maximum opening point (A) the mandible rises (3) and returns to the starting position (O, R) or may be pushed forward (4) to maximum protrusion (P) and from here sliding back with teeth in contact (5) returns to the starting point (O, R).
Posselt’s Diagram
- Hyoid Bone
Anatomy
A single, median, mobile bone shaped like a horseshoe; it is
located in the neck, above the larynx and below the mandible, with which it helps form the skeletal floor of the oral cavity. It is connected, besides the mandible and the laryngeal skeleton, to the temporal bone, sternum, sternal end of the clavicle and scapula. These connections are made through ligaments and muscles. The bone consists of a body that has four appendices: two greater horns and two lesser horns. The body appears as a transversely oriented plate; it has three surfaces: superior, anterior, and posterior, and three borders: inferior, anterior, and posterior. On the superior surface, there are two fossae for insertion of the geniohyoid muscles; on the anterior surface insert the mylohyoid and stylohyoid muscles; the posterior surface faces backward and downward and presents a pronounced concavity. The inferior border gives insertion to the sternohyoid and omohyoid muscles; the anterior border partially attaches the mylohyoid muscle; on the posterior border the median thyrohyoid ligament attaches. The greater horns are posterior prolongations of the body and ascend tapering, then widen again at the tips. They have a superior surface for the insertion of the hyoglossus muscle, an inferior surface for the insertion of the thyrohyoid muscle, a medial border for the attachment of the thyrohyoid membrane and the middle pharyngeal constrictor muscle, and a lateral border for the insertion of the hyoglossus muscle. At the apex of the greater horns are the lateral thyrohyoid ligaments. The lesser horns originate at the junction where the body continues into the greater horns and, for a variable length, ascend. They are connected to the styloid processes of the two temporal bones by the stylohyoid ligaments.
Articular Physiology
The hyoid bone serves as the support point for mandibular opening movements, participates in swallowing, phonation, and breathing, intervenes in the positioning of the skull and scapula; moreover, through its direct musculo-fascial connections with skull, mandible, sternum, and scapula, and indirectly through muscles running from scapula and sternum cranially towards cervical vertebrae and skull, and caudally towards thoracolumbar vertebrae and pelvis, it can influence and be influenced by all body regions. Therefore, it plays a pivotal role in the functional balance within the stomatognathic system and its relation to the rest of the body.
1.4 Masticatory Muscles
The muscles that produce various mandibular movements, as well as other functions, are defined as masticatory muscles. These muscles are classified based on the movements they produce in the mandible along with their contralateral counterpart. They are:
- Elevator muscles
- Depressor muscles
- Protruder muscles
- Retruder muscles
- Abductor muscles
- Adductor muscles
Elevator muscles
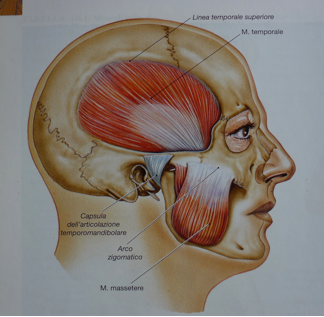
They include the masseter, temporalis, and medial pterygoid muscles. They act during mandibular closing phase.
The masseter is a rectangular muscle attached superiorly to the zygomatic arch, inferiorly to the masseteric tuberosity of the lateral mandibular ramus. Its function is to elevate the mandible and create tension in the dental arch occlusion.
The temporalis is a large fan-shaped muscle that extends from the lateral skull surface downward and, passing medially to the zygomatic arch, inserts via a strong tendon onto the coronoid process of the mandible. The posterior fibers pull the mandible backward helping to reposition the condyle in the articular cavity, and the anterior fibers elevate the mandible.
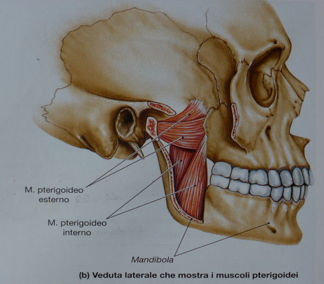
The medial pterygoid originates from the pterygoid fossa and maxillary tuberosity and inserts onto the pterygoid tuberosity near the internal mandibular angle. Its function is to elevate the mandible.
Depressor muscles
These are considered physiological flexors: digastric, lateral pterygoid, mylohyoid, and geniohyoid muscles.
The digastric forms an arch connecting the mandible to the mastoid process via two bellies united by an intermediate tendon fixed to the hyoid bone. The anterior belly, together with the mylohyoid and geniohyoid muscles, using the hyoid bone as a fixed point, lower the mandible.
Protruder and retruder muscles
The lateral pterygoid is the main protruder. The posterior fibers of the temporalis, aided by the digastric, perform retrusion.
The lateral pterygoid is located in the infratemporal fossa, medial to the mandibular ramus. It originates from the greater wing of the sphenoid with the superior head, and from the lateral plate of the pterygoid process with the inferior head, inserting on the neck of the mandibular condyle. When contracting with the opposite side, it moves the mandible forward; if contracting only on one side, it moves the mandible forward and to the opposite side.
Abductor and adductor muscles
The muscles producing abduction and adduction are the medial pterygoids and sternocleidomastoids. The mandible moves toward the contralateral side of the contracting muscles. Adduction can be passive or active, the former through muscle relaxation, the latter through contraction of muscles on the side toward which the mandible moves.
- Teeth
Teeth are organs primarily intended for the first phase of digestion, that is,
mastication, by which food is thoroughly crushed. Teeth are classified as incisors, canines, premolars, and molars based on their shape. Each tooth consists of two parts: the CROWN, located above the gum, and the ROOT, embedded in the alveolar process; the demarcation line between the two is called the “neck of the tooth” which separates two different tissues: enamel covering the crown and cementum covering the root.
The innermost portion of the tooth is a cavity called the PULP CHAMBER. This is also known as the root canal, which ends at the root apex with a hole called the apical foramen. Inside the pulp chamber is contained the DENTAL PULP.
Each tooth crown has several surfaces: a mesial surface facing the preceding tooth in the arch; a distal surface facing the next tooth; a vestibular surface corresponding to the outer surface; a lingual surface corresponding to the inner surface; and an occlusal surface corresponding to the surface contacting the opposing arch.
Teeth are supported in the mouth by a structure called the periodontium composed of:
- gingiva (mucosa part surrounding the neck of the tooth covering underlying bone)
- periodontal ligament (a complex system of fibers that binds
the tooth to its socket in the bone)
- cementum (external covering of the tooth root)
- alveolar bone (internal wall of the socket, which is the
site of the tooth in the bone).
Mammals and humans have two dentitions: a primary or deciduous (milk) dentition consisting of 20 teeth divided into two arches, 10 teeth in the upper arch and 10 in the lower, and a secondary permanent dentition which replaces the first and consists of 32 teeth, 16 per arch. The first teeth to appear in a child's mouth, around the 6th to 8th month of life, are the lower central incisors, followed at 8-10 months by the upper incisors; at 10-12 months the lower lateral incisors; around 16 months the first molars begin to erupt; around 18 months the canines; and around 20 months the second molars. Normally, dentition is complete between the 6th and 30th month. Sometimes tooth eruption may be delayed or early. If eruption is significantly delayed, one should consider general growth disorders causing slowed dental development; these can be due to calcium or phosphorus imbalance, vitamin deficiency, or in pronounced delays, endocrine disorders (hypothyroidism, hypothyroidism, rickets, etc.). Tooth loss follows the same chronological order as eruption; roots undergo progressive atrophy until the unsupported crown falls out. The timing of deciduous tooth loss corresponds to the eruption of permanent teeth.
CHAPTER 2
POSTURE
Posture can be understood as the position of the body in space and the spatial relationship between skeletal segments, aimed at maintaining balance, both in static and dynamic conditions, influenced by neurophysiological, biomechanical, psychoemotional, and relational factors.
It follows that posture can be studied through each of the following interpretative models: psychosomatic model, neurophysiological model, biomechanical model.
2.1 THE PSYCHOSOMATIC MODEL
The first formulations by W. Reich and later by A. Lower date back to the 1920s, on the profound relationship between psyche and soma, between character structure and muscular structure.
In his early writings, Reich, a physician and psychoanalyst, a student of Freud, progressively asserted the functional identity between psychic and somatic processes, relating character structure to the body structure of the person. The tensions accumulated in the body and the enactment of attitudes aimed at blocking one’s emotions give rise, according to the scholar, to a dual armor.
This is a character armor, understood as the set of psychic and behavioral attitudes characteristic of an individual, which corresponds somatically to a muscular armor.
These attitudes function as a defense apparatus against both internal and external stimuli perceived by the subject as threatening, aimed at avoiding feelings of anguish. Also described in orthopedics as “psychogenic myotensive state,” chronic muscle tension represents perhaps the most evident process through which the Ego expresses its emotional experiences in the body. It can therefore be stated that the muscular structure also reveals an individual’s personal history. The relationship between posture and personality is now supported by numerous scientific studies from scholars of various schools. It is important to remember that to represent each individual in their psychomotor unity, alongside muscular-tensive and postural aspects, it is essential to also consider psycho-neuroendocrine factors, viewed as the mediating and modulating system between psychic-emotional components on one side and organic-biological factors on the other. The formation of the bodily armor occurs through an increase in basal tone, i.e., excessive tension in the contractile portion of muscle fibers. If this persists over time, the connective tissue portion is also affected, causing actual shortening of the muscular system which will lead to alteration of the normal articular sequence. Thus, an emotionally-originated myotensive state may evolve into a biomechanical problem.
THE NEUROPHYSIOLOGICAL MODEL
The tonic postural system, regulator of muscle tone, is a cybernetic system within which a complex series of psycho-neurophysiological processes occur. In this system, incoming information from specific posture receptors (foot, eye, stomatognathic system, skin, musculoskeletal apparatus, etc.) conditions the output, i.e., muscle tone. However, this output conditioning is itself the result of processing of inputs by neuropsychological and experiential processes. Therefore, postural imbalance does not necessarily indicate a primary problem at the sensory input level but may be linked to improper integration of the central system: cortical centers identify static or dynamic goals while subcortical centers, using a mapping defined as “body schema,” execute strategies. Cortical centers identify the “what,” subcortical centers the “how.”
Furthermore, subcortical centers regulate basal tone through the gamma circuit. Since the “what” is prioritized over the “how,” the subjective representation of the body schema determines the quality of muscular use: the less well represented the body schema, the more the muscular system is used in excess tension, in co-contraction of unnecessary muscles for the action up to organizing compensatory moments, where anatomically assigned muscles to a given action are substituted by others (emerging abilities). Subcortical centers are also involved in defensive strategies aimed at preserving life through muscle contraction mechanisms distinguishable as “physiological” and “functional.”
Muscle contraction, depending on force/time variables, determines residual muscle shortening: the shorter the contraction time and force, the less residual shortening; the greater the force and especially time, the greater the residual shortening. Muscle shortening and consequent body asymmetry are not only found in people with orthopedic pathology/symptoms but are present in all humans, induced by automatic muscle contractions in response to an event. In the following, “physiological” means muscle contraction mechanisms used by every human as a response to an event/stimulus; “functional” means muscle contraction mechanisms used by every human but with subjective variability in quantity and quality answering the question “what I need.”
Both mechanisms are controlled by subcortical centers. Subcortical centers are atavistic centers in the phylo-ontogenetic evolution of humans and have among their primary tasks to adopt strategies useful for life preservation.
Physiological Mechanisms
They are muscle reactions in sustained contraction following an orthopedic traumatic event.
Example: accidental event and ankle sprain.
Subcortical centers send, via the gamma motor neuron, a contraction message to all periarticular muscles to immobilize the joint. This contraction lasts until the intra-articular damaged structures are repaired. The contraction duration is proportional to the damage; consequently, so is the residual muscle shortening.
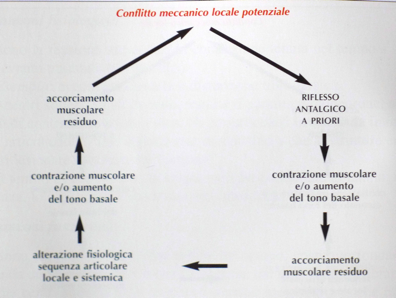
Functional Mechanisms
They are sustained muscle contractions, fundamentally consisting of more or less significant increases in basal tone and always activated by subcortical centers via the gamma motor neuron, aimed at attenuating and/or eliminating present pains (retroactive antalgic reflex) or preventing latent pains from manifesting (proactive antalgic reflex). Sustained muscle contraction over time, as long as it does not cause structural conflicts, has an analgesic effect. In safeguarding life, subcortical centers have only one time: “here and now.”
Pain and/or functional impairment are perceived as “death” and avoidance strategies must be adopted. In this perspective:
“Retroactive Antalgic Reflex”
It represents the extreme defense strategy to prolong life as much as possible. People in acute pain often assume twisted postures but, as patients say, they feel somewhat better this way.
This defensive strategy is useful immediately but, if prolonged, will cause further mechanical conflicts.
Physiological mechanisms and the retroactive antalgic reflex intervene only at some moments of life and alone are insufficient to explain the sum of shortenings and asymmetries present in the body. These are mainly caused by:
“Proactive Antalgic Reflex”
It is a permanently active reflex aimed at preventing latent pains/mechanical conflicts from manifesting. Progressive muscle shortening, as long as it does not cause conflicts, prevents the unmasking of musculoskeletal discomfort. Subcortical centers use the muscular system distributing shortenings to systematically alter joint sequences avoiding local conflicts. The proactive antalgic reflex manifests also through posture adoption or movement, forcing the person to motor choices. These coercions are initially unconscious: one “feels” the need/desire to move or position in space a certain way. If muscular shortening modifications become more important, motor coercions become consciously aimed at avoiding discomfort onset. If the systemic muscular shortening mechanism persists over time, local conflicts can arise creating a self-feeding circuit where both antalgic reflexes coexist.
In conclusion, the human body, in living, cannot adhere to the anatomical model also due to subcortical protective systems that allow living the best “here and now” possibilities, sacrificing the “later.” For this, centers use the muscular system increasing basal tone and/or muscle contraction creating an analgesic effect; if tension increase occurs long enough, muscle shortening results. This causes:
- Systemic muscle shortenings;
- Analytical muscle shortenings of some dominant groups, by force vector, compared to others;
- District and systemic alterations of the physiological skeletal articular sequence.
THE BIOMECHANICAL MODEL
The biomechanical model analyzes how the musculoskeletal system “organizes” itself in static and dynamic conditions. In statics, postural imbalances are evident by loss of the physiological articular sequence of the various skeletal segments in three spatial planes; in dynamics, by the inability to perform movement using muscular forces optimally. To ensure axiality of skeletal segments and physiological joint movement, muscular forces must be balanced. Otherwise, the points of application of muscular force vectors, their moments, and load distribution on skeletal segments change. Regardless of primary disturbing elements and initial perturbation type, postural alteration results from the interaction between the “complex” muscular and “complex” skeletal systems, creating a functional interrelation “musculoskeletal complex system.” A localized perturbation causes initial misalignment and thus articular imbalance followed by muscle contraction with a stabilizing function, but vice versa, proper articular sequence organization depends on muscular tension balance. Low-intensity balance (muscle tone) guarantees coexistence of good stability and good joint mobility, creating conditions so the musculoskeletal system operates “at the edge of chaos,” the area where static and dynamic elements express the best structural possibilities. If force balancing occurs at high intensity, skeletal axiality is still possible, but movement will require more energy. Movement becomes disharmonious and skeletal components undergo more stress. Static elements prevail over dynamic ones and the system, moving away from the “chaos margin,” becomes rigid. High-intensity balance (increased basal tone) causes over time a vector imbalance favoring dominant muscular forces and reorganization of a new adaptive equilibrium at the price of segmental skeletal displacements.
Movement will be limited or replaced through mobilization of other joints.
CONCLUSIONS
The three neuromuscular, psychosomatic, and biomechanical systems use the muscular system to achieve their goals.
They also interact and are interdependent: whichever system is primarily involved in imbalance, the others must adopt adaptive strategies to safeguard function as best as possible. The action on the muscular system is expressed through increased basal tone and district and systemic muscle contraction. If muscle contraction and/or basal tone increase persist long enough, the connective portion of muscle fibers is involved, resulting in residual shortening that causes misalignment of the physiological articular sequence.
This in turn causes muscle contraction and basal tone increase creating a self-feeding circuit.
CHAPTER 3
OCCLUSION AND MALOCCLUSION
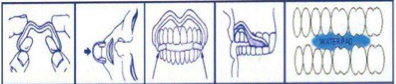
3.1 OCCLUSION
Occlusion is generally defined as any relationship between the arches whenever even some of their respective teeth come into contact, either with the mandible at rest or during functional movements of the temporomandibular joints. Normally, in the rest position, teeth do not contact but the two arches are separated by a free space (freeway space). In a properly functioning stomatognathic apparatus (habitual physiological occlusion), when the two dental arches occlude (swallowing, final chewing phase), they do so in the most stable position, i.e., the one characterized by the maximum number of contacts between antagonistic elements (maximum intercuspation position), with uniform distribution of masticatory loads, respecting the periodontal structures, masticatory muscles in normal tone, and temporomandibular joints. This equilibrium situation is therefore linked to several interrelated factors:
- The shape of the dental arches
- The temporomandibular joints
- The masticatory muscles
- Neuromuscular control
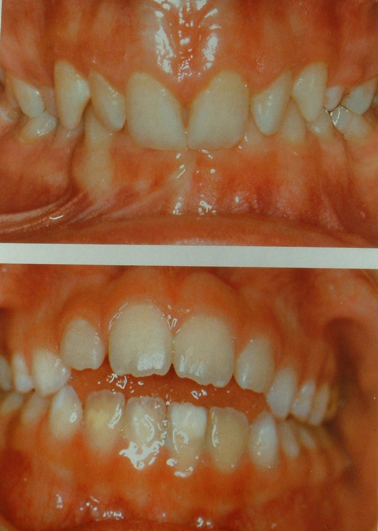
Any variation in one of these components causes an imbalance which, when exceeding the individual’s compensatory capacity (highly variable person to person), results in a pathological condition. Correct occlusion meets the following three parameters in maximum intercuspation position (ICP):
1) Upper teeth are positioned outside the lower teeth by about half a cusp for molars and premolars.
2) Upper incisors cover the lower incisors by about 2 mm.
3) The first lower permanent molars are anterior by half a cusp relative to the first upper molars; therefore, all teeth, upper and lower, touch two antagonist teeth, interlocking stably.
Optimal occlusion is associated with harmonious action of masticatory muscles with minimal muscular effort. Conversely, occlusal alterations require additional stabilizing muscular effort. In conclusion, normocclusion is not limited to achieving good aesthetics and good dental engagement but goes beyond. According to many authors, “achieving normocclusion means obtaining static and dynamic harmony among basal-neuromuscular structures, dental structures, and soft tissues.” This means respecting not only tooth function but also that of all interconnected muscles.
3.2 MALOCCLUSION
Malocclusion is present when dentition is incorrect, i.e., when there is abnormal dental alignment.
It should be noted that some defects tend to resolve or lessen spontaneously, while others require early interception. This is the realm of “interceptive orthodontics,” defined as:
- Early therapy aimed at prevention.
- Correction of initial malocclusion to prevent worsening.
- Identification, evaluation, and control of mechanisms worsening initial malocclusion.
Malocclusion can be linked to defects confined to a single arch (intra-arch) and/or to defects in the relationships between the two dental arches (inter-arch). There are even severe dental malocclusions with individually perfect arches; this due to displacement of one arch relative to the other.
Intra-arch defects
Causes: alteration of tooth number and shape, agenesis, rotations, dislocations, inclusions of teeth.
Manifestations: crowding and misalignments (when space is lacking)
Interdental spacing (in space excess)
Inter-arch defects
Defects in arch relationships manifest in three spatial planes and are classified accordingly:
- Frontal plane
(e.g., open bite, deep bite)
- Horizontal plane
(e.g., constricted bite, crossbite, bite inversion)
- Sagittal plane
(e.g., Class II and III)
3.2.1 Alterations in the frontal plane
Open bite
There is a large vertical space between upper and lower anterior teeth. Besides losing lip seal, an infantile swallowing pattern is established, with the tongue pushing violently between the two arches, probably to obtain closure allowing a depression useful for swallowing. Main causes of open bite are pacifier use and thumb sucking.
Deep bite
Upper incisors excessively cover lower ones, sometimes completely. If upper incisors are flexed anteriorly creating excessive transverse space (overjet) between them and lower incisors, this causes loss of lip seal and forces the tongue to abnormal work during each saliva swallowing. If upper incisors are bent posteriorly, this may influence mandibular moments forcing it to stay further back.
3.2.2 Alterations in the horizontal plane
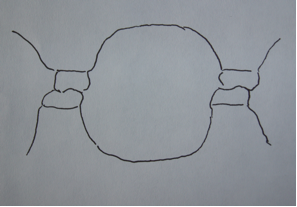
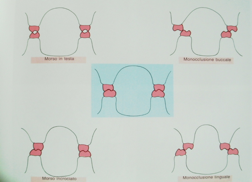
In transverse plane alterations, the relationships between upper and lower molars are altered: upper molars, which should be more external than the corresponding lower ones, often are not. Included here is:
Crossbite
teeth on one or both sides occlude inversely to normal (upper molar remains more internal rather than more external than the lower). Unilateral crossbite is almost always accompanied by lateral mandibular and chin displacement toward the crossing side. In these cases, overload of the joint on the deviation side (the condyle is compressed toward the articular cavity) and asymmetric muscle contracture are common.
In bilateral crossbite, symmetry may be preserved but pathological occlusion limits mandibular functional movements causing facial muscle spasms (contractions).
Underbite
Typical in classic Class III malocclusions. In this case, there is a transverse space between upper and lower incisors due to mandibular protrusion (lower incisors anterior to upper ones).

Lip seal and normal swallowing and chewing function are also compromised here. Contractions and inversions may affect one or more teeth up to the entire upper arch; in this case, transverse plane alteration is associated with sagittal plane alteration grouping.
- Alterations in the sagittal plane
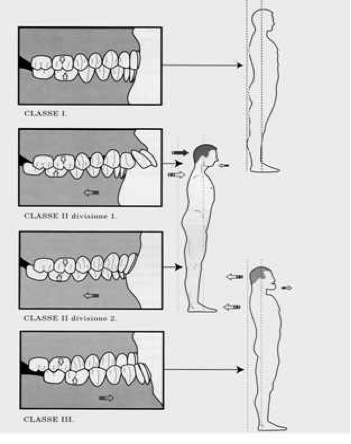
In the sagittal plane, skeletal and dental malocclusions are classified according to Angle’s system:
The position of the first permanent molar of the lower dental arch relative to the first permanent molar of the upper arch determines the malocclusion classification. The normal occlusion condition is called Class I, or neutro-occlusion. In this case, the mesiobuccal cusp of the first upper permanent molar occludes in the mesiobuccal groove of the first lower permanent molar. Malocclusion occurs when the mesiobuccal cusp of the upper molar is positioned either anterior or posterior to the mesiobuccal groove of the lower molar. In the first case, it is a Class II malocclusion (distal occlusion), in the second case, it is a Class III malocclusion (mesial occlusion).
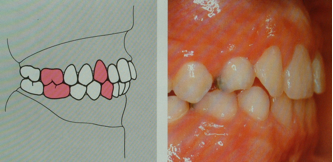
Angle’s Classification of Malocclusion:
A – Class I. Normal occlusion.
B – Class II. The mesiobuccal cusp of the first upper molar is positioned anterior to the mesiobuccal groove of the first lower molar.
C – Class III. The mesiobuccal cusp of the first upper molar is positioned posterior to the mesiobuccal groove of the first lower molar.
Class II Malocclusion
This malocclusion involves a retrusion of the mandible relative to the maxilla, creating a distal occlusion. It can be subdivided into two divisions:
- Division 1: Proclined upper incisors, increased overjet.
- Division 2: Retroclined upper central incisors, deep bite.
Class III Malocclusion
This is characterized by mandibular protrusion or maxillary retrusion, leading to an anterior crossbite and sometimes an underbite. It often has a genetic basis and can affect function and aesthetics significantly.
CONCLUSIONS
The relationship between occlusion and posture is complex and multifactorial, involving dental, muscular, articular, and neurological components. Malocclusions can contribute to postural alterations, but their role is often integrated within a broader context of systemic factors. Thus, multidisciplinary assessment and intervention are fundamental in cases where occlusal and postural disorders coexist.
- DESCENDING ALTERATIONS FOLLOWING BAD DENTAL OCCLUSION
All the postural imbalances seen may in turn generate the onset of orthopedic pathologies (scoliosis, low back pain, neck pain, etc.) that can be defined as secondary to a primary pathological involvement of the stomatognathic system and are usually grouped into three categories:
- Alterations on the sagittal plane
- Alterations on the frontal plane
- Alterations on the horizontal plane
Before addressing the following alterations, it is necessary to remember the key role of the hyoid bone in the balance between occlusion and posture. The hyoid bone, through its direct connections with the skull, mandible, sternum, and scapula and indirect connections through muscles that run cranially from scapula and sternum towards the cervical vertebrae and skull, and caudally from scapula towards thoraco-lumbar vertebrae and pelvis, is able to influence and be influenced by all body regions. The hyoid muscles therefore participate in the strategies that the system implements to achieve its goals, both in static and dynamic conditions. If the hyoid muscles develop excessive tension and subsequent shortening, besides causing local and systemic skeletal misalignments, they can cause swallowing and phonation disorders.

- Alterations on the sagittal plane
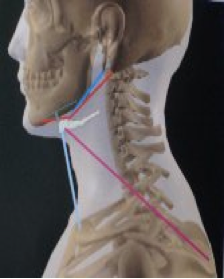
The Class I skeletal corresponds to physiological normality, i.e.: head "in centric" position relative to the cervical spine, mandible "in centric" relative to the skull, and tongue "in centric" on the palate. These three "centric relations," being interdependent, must be sought and evaluated simultaneously.
Since these are, in turn, closely dependent on overall posture,
the necessity for a complete postural examination becomes evident.
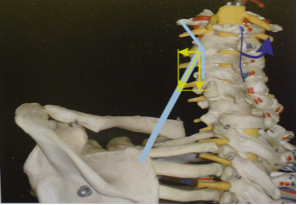
In Class II basal type, we have: retrusion of the mandible relative to the maxilla (corresponding to a high posterior displacement of the condyles relative to the temporal fossae with consequent steeper condylar trajectories), tongue interposed anteriorly at rest and during swallowing, inefficient lip seal because the lower lip is posteriorized compared to the upper one. This situation affects cervical posture and, consequently, overall posture. For example, there may be a predominance of posterior muscle tone, extension of the occiput relative to the atlas (the head "opens" on the neck), cervical spine straightening but with concentration of hyperlordosis in the atlanto-occipital segment.
In Class III, we have: protrusion of the mandible relative to the maxilla (condyles positioned anteriorly and inferiorly, thus gentler condylar trajectories), tongue in a low position resting on the mandible with consequent incompetence of the lip seal because here the lower lip is anteriorized relative to the upper one. Based on individual reactions, for example, there may be predominance of anterior neck musculature, occiput in flexion relative to the atlas (the head "folds" toward the chest "closing" on the neck), with alteration of the physiological cervical lordosis which tends to concentrate in the lower segment then straighten or even invert in the upper segment.
- Alterations on the frontal plane
In this plane, a lateral deviation of the mandible can influence the harmony of the scapular and pelvic girdles, causing a series of adaptations of the tonic-postural system.
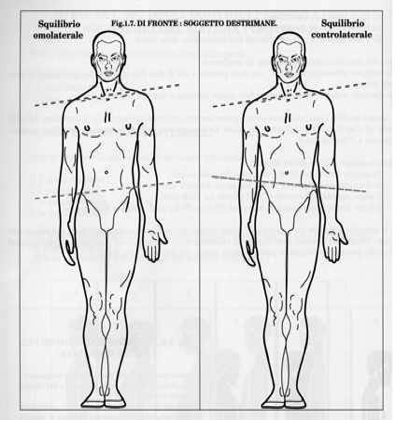
- Alterations on the horizontal plane
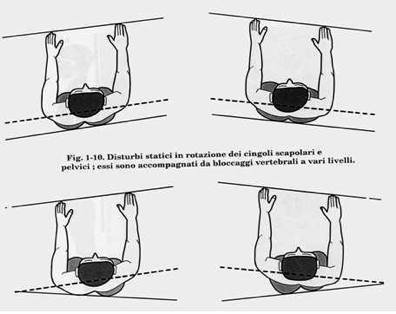
On the horizontal plane, mandibular deviation can induce
rotations of the scapular or pelvic girdle, ipsilateral to the side of the
deviation or create a crossed system with anteriorization of the
scapular girdle on one side and the pelvic girdle on the opposite side.
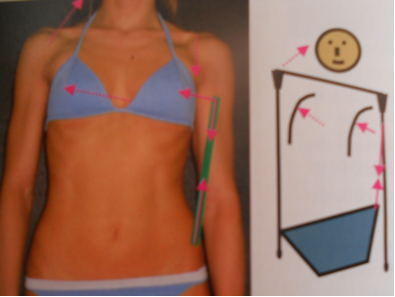
- FRONTAL PLANE DEVIATIONS AND ROTATIONS
In the presence of a lateral displacement of the mandible during closure, there is a state of suffering of the muscles involved with the displacement itself (for example, ipsilateral posterior temporalis, external pterygoid and contralateral anterior temporalis, internal pterygoid).
The repercussions on the neck musculature may involve:
- the ipsilateral upper trapezius and contralateral sternocleidomastoid, so that the head will flex on the side of the deviation approaching the shoulder, which will be higher than the contralateral one.
- The levator scapulae and ipsilateral scalenes cause vertebral convexity on the same side from C1 to C7 and rotate the vertebral bodies ipsilaterally. Under these conditions, the cervical spine will be deviated, and compensatory curves will inevitably form at thoracic and lumbar levels. The involvement of the spine reflexively causes other muscular imbalances such as in the latissimus dorsi.
- the latissimus dorsi: shortening of this muscle, having many insertion points, produces various skeletal effects. Schematically, two main patterns “A” and “B” can be distinguished which often appear mixed rather than pure.
Pattern A
This pattern mainly involves the latissimus dorsi bundles from the iliac crest to the humerus, which by approximating the hemipelvis and the shoulder directly cause lowering of the shoulder and elevation of the hemipelvis and, as a mechanical result, the ipsilateral lateral concavity. These bundles are also responsible, by mechanical consequence, for the contralateral thoracic lateral convexity and contralateral high shoulder.
If mechanical results prevail, the spinal curve will show a wide-range scoliosis with contralateral convexity, which is actually a consequence of the ipsilateral concavity caused by the approximation of shoulder and hemipelvis.
The latissimus dorsi inserts on the spinous processes from D12 to D7 and, through the thoracolumbar fascia, on the costiform processes of lumbar vertebrae. The quadratus lumborum, besides the twelfth rib, inserts on the costiform processes of the first three lumbar vertebrae. Their force line is thus able not only to elevate the hemipelvis but also to pull the vertebrae from L5 to D7. The latissimus dorsi and quadratus lumborum oppose the mechanical result induced by hemipelvis elevation maintaining or even creating an ipsilateral convexity. In this case, a double curve results where latissimus dorsi and quadratus lumborum are directly responsible for lumbar and lower thoracic vertebral convexity by direct traction on vertebrae, and for upper thoracic vertebral concavity as a result of shoulder and hemipelvis approximation.
Pattern “B”
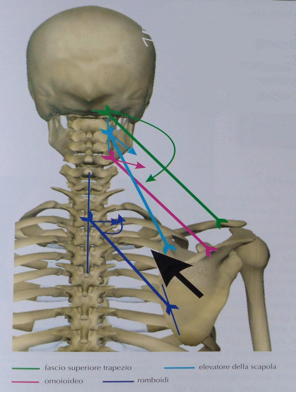
This pattern is characterized by the combined action of the upper latissimus dorsi bundles and muscles dominant in shoulder stump elevation. Together, these muscles produce an overall result that elevates the scapula in adduction and the clavicle. If the omohyoid is involved, the hyoid bone will be deviated laterally.

The thoraco-humeral bundles of the latissimus dorsi cause thoracic lateral convexity in the lower quadrant while the lower bundles elevate and rotate the hemipelvis posteriorly.
The thoracic lateral convexity is also a mechanical consequence of the elevation of the shoulder stump, directly caused by rhomboids and middle trapezius bundles that, by elevating and adducting the scapula, can produce ipsilateral convexity of the thoracic vertebrae thoracic vertebrae.
The vertebral convexity will affect the upper-lateral quadrant of the thorax and will involve the serratus anterior which increases its tension trying to prevent scapular adduction and elevation. However, being under-dominant, the scapula becomes a fixed point and its traction manifests on the ribs (a mobile point) which will shift laterally.
The associated pattern will potentially have the following skeletal characteristics on the same hemibody, not necessarily all present, due to direct muscle action:
- elevated and adducted scapula
- ascending clavicle
- lateralization of the hyoid bone
- thoracic lateral convexity in the upper quadrant (above D7)
- thoracic lateral convexity in the lower quadrant (below D7)
- elevation of the hemipelvis
- posterior rotation of the hemipelvis

Blue arrows: overall result of the action of the shoulder stump elevators and upper latissimus dorsi bundles.
Pink arrows: action of the costo-humeral bundles of the latissimus dorsi.
Green arrows: action of the lower bundles of the latissimus dorsi.
Light blue arrows: action of the middle trapezius bundles and rhomboids.
Yellow arrows: action of the serratus anterior.
CHAPTER 5
EVALUATION AND DIAGNOSIS OF POSTURAL ALTERATIONS DUE TO DYSFUNCTIONS OF THE DENTAL OCCLUSAL PLANE
5.1 INTRODUCTION
Disorders and dysfunctions in the cranio-cervico-mandibular district are a complex of still poorly understood pathologies that have been increasing in number and severity in recent years. Recent epidemiological studies indicate that 50-60% of the population show signs and/or symptoms of functional alteration of the masticatory system and related structures, and many show altered posture compared to physiological posture. It is generally accepted that the etiology is often multifactorial, with various predisposing, precipitating, and perpetuating factors. Predisposing factors refer to all components increasing the probability of the pathology appearing; precipitating factors are events causing onset; perpetuating factors slow healing or accelerate progression. It is therefore fundamental to recognize every sign and symptom of temporomandibular joint dysfunction and related structures, weighing importance and need for treatment. This assessment should not rely solely on medical diagnosis but should especially consider the specific health condition of the patient according to a biopsychosocial model, which relates structural damage with problems it causes in other health areas proposed by the ICF. This model allows construction of a general descriptive framework of the patient's health status, guiding identification of possible corrective and rehabilitative intervention areas and positive/negative prognostic factors related to the person or physical and social environment. Furthermore, a properly conducted functional evaluation allows better exclusion of contraindications to treatment and/or identification of patients to be referred to other health professionals or multidisciplinary approach. Finally, as with any medical-health act, it is essential to obtain patient consent to the treatment plan after detailed information on diagnosis and prognosis, expected benefits, possible alternatives, risks, and therapy complications.
Effectiveness and success of treatment depend on correct diagnosis, which can be formulated only after detailed anamnesis and accurate clinical examination.
- ANAMNESIS
Collecting the patient's clinical history is a fundamental moment in conducting a clinical exam: it allows critical information relevant to etiopathogenesis to be detected, and helps build diagnostic and prognostic hypotheses. This relational data acquisition process is very complex and, although based on a strict methodology, constitutes an art perfected only through practice and experience. The main phases of anamnesis acquisition are:
-Acquisition of demographic data
(name, surname, age, occupation, hobbies, sports, etc.)
-Reason for consultation and description of the problem (description of current disorder, precise localization of painful area, when and how it started, any triggering factors, evolution of disorder).
-Past general and specific pathological anamnesis (surgical interventions, pharmacological therapies, relevant diseases)
-Current state (description of pain, VAS scale, what worsens/improves pain symptoms, difficulties in performing certain daily and work activities)
-Patient expectations (what they expect to receive from the therapeutic intervention).
For each of these moments, precise questions must be asked, respecting the patient's socio-cultural condition and particular emotional experience. An interview can be structured using questionnaires such as the “Research Diagnostic Criteria for Temporomandibular disorders”, introduced for the first time in 1992 by Dworkin and LeResche, constituting the current international classification for cranio-mandibular disorders.
ON PAIN:
Graded Chronic Pain Scale
Please read each question and respond accordingly. For each of the
questions below circle only one response.
1. How would you rate your facial pain on a 0 to 10 scale at the present time, that is right now, where 0 is "no pain" and 10 is "pain as bad as could be"?
Pain as bad No pain as could be
0 1 2 3 4 5 6 7 8 9 10
2. In the past six months, how intense was your worst pain rated on a 0 to 10 scale where 0 is "no pain" and 10 is "pain as bad as could be"?
Pain as bad No pain as could be
0 1 2 3 4 5 6 7 8 9 10
3. In the past six months, on the average, how intense was your pain
rated on a 0 to 10 scale where 0 is "no pain" and 10 is "pain as bad as
could be"? [That is, your usual pain at times you were experiencing pain].
Pain as bad No pain as could be
0 1 2 3 4 5 6 7 8 9 10
4. In the past six months, how much has facial pain interfered with your daily activities rated on a 0 to 10 scale where 0 is "no interference" and 10 is "unable to carry on any activities"? Unable to No carry on interference any activities
0 1 2 3 4 5 6 7 8 9 10
5. In the past six months, how much has facial pain changed your ability to take part in recreational, social and family activities where 0 is "no change" and 10 is "extreme change"?
Unable to No carry on change any activities
0 1 2 3 4 5 6 7 8 9 10
6. In the past six months, how much has facial pain changed your ability to work including housework) where 0 is "no change" and 10 is "extreme change"?
Unable to No carry on change any activities
0 1 2 3 4 5 6 7 8 9 10
7. About how many days in the last six months have you been kept from your usual activities (work, school or housework) because of facial pain?
____Days
ON FUNCTION:
Jaw Function Questionnaire
Jaw Disability Checklist
What activities does your present jaw problem prevent or limit you from doing?
No Yes
Chewing 0 1
Drinking 0 1
Exercising 0 1
Eating hard foods 0 1
Eating soft foods 0 1
Smiling/laughing 0 1
Sexual activity 0 1
Cleaning teeth or face 0 1
Yawning 0 1
Swallowing 0 1
Talking 0 1
Having your usual facial appearance 0 1
- PHYSICAL EXAMINATION
An accurate clinical examination is fundamental to record all useful information for diagnosing the type of disorder and to establish the severity of the pathology also in relation to symptoms reported by the patient. This information is decisive to elaborate an adequate treatment plan guided by the needs of the individual case and to establish the prognosis in the short and long term; the examination is based on the concepts of:
- inspection,
- palpation,
- auscultation,
- evaluation of extra and intraoral structures
- postural exam.
Below I will propose the fundamental diagnostic test to define whether the cause of the postural alteration and pain is stomatognathic in nature, particularly occlusal, or not:
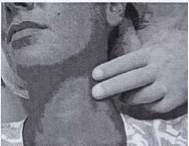
PRINCIPAL DIAGNOSTIC TEST ON THE ROLE OF OCCLUSION IN POSTURAL ALTERATIONS
(Cotton rolls test or hydrodynamic bite test with communicating vessels).
Cotton rolls:
Insert two cotton rolls between the teeth (or two neoprene strips 5-6 mm thick). Have the patient walk and swallow several times (5-6 swallows, about twenty seconds) and verify induced postural changes. If posture improves, it can be assumed that the mouth is a triggering factor (descending syndrome), if it worsens, beware: we might be facing a compensatory occlusion of another cause (eyes, pelvis, short limb, etc.) (ascending syndrome). In these cases it is appropriate to combine postural therapy with occlusal therapy, possibly with pre-made bite splints (mioset).
Hydrodynamic bite:
This type of bite, by preventing the patient's habitual dental occlusion, reprograms mandibular movement into muscular equilibrium (reprogramming occurs at every occlusion). If tooth position interferes with posture, significant variations of overall posture, realignment of cervical vertebrae and repositioning of the hyoid bone will be observed. Subjectively, the patient may report sensations of well-being at the cranio-cervical tract but also in underlying body districts. The hydrodynamic bite is used for examination and is not a therapeutic tool; the bite has the property of floating the mandible so that the patient's tooth position and size do not constrain mandibular position at occlusion. It represents a closed system that levels forces so pressure is the same on every tooth surface. The muscles controlling mandibular movements are thus freed from occlusion and intercuspidal proprioceptive system.

If these tests are positive, in a causal logic, it becomes desirable to refer the patient to a gnathologist or dentist.
Regarding the general objective examination of the stomatognathic and postural apparatus, the following will follow:
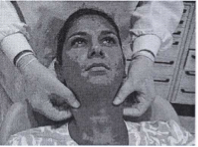
- INSPECTION
Extraoral inspection will aim to identify the possible presence of swellings, redness, scars and facial asymmetries or skeletal conditions that may represent unfavorable morphological conditions.
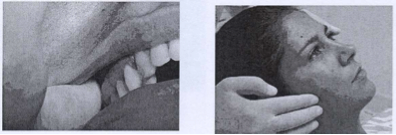
Intraoral inspection will be useful to identify any inflammatory and infectious conditions; furthermore, a baseline examination of the patient's dentition will be necessary (noting any missing teeth, deviations, inclinations) and the occlusal relationships on the sagittal plane (class I, II, III, overjet), transverse (crossbites) and vertical (measuring the distance between mandibular and maxillary arches at maximal intercuspation and possible overbite).
5.3.2 PALPATION
Palpation is commonly conducted on muscular and articular structures of the affected district to identify the pain source. Focusing on the stomatognathic apparatus we evaluate:
5.3.2.1 Muscles:
Normally, function or palpation of a muscle does not evoke pain. If it does, tissue compression due to trauma or fatigue may be inferred. During examination, pain intensity must be assessed and recorded using the VAS scale. Possible trigger points (areas of hypersensitivity associated with referred myofascial pain) must be evaluated.
Temporalis: palpation of vertical fibers of the anterior area is performed above the zygomatic arch anterior to the TMJ, transverse fibers of the middle area are palpated above the TMJ area, horizontal fibers of the posterior area are palpated above and slightly behind the ear. The tendinous insertion on the coronoid process is palpated by placing the index finger inside the mouth at the anterior border of the mandibular ramus upwards.
Masseter: the deep portion is palpated on the zygomatic arch just in front of the tragus sliding fingers downward 2-3 cm. The superficial portion is palpated externally and bilaterally sliding fingers from the zygomatic arch to the lower border of the mandibular ramus. The superficial masseter can also be palpated by pinching externally at the mandibular ramus.
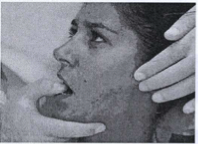
Internal Pterygoid: palpation is performed with the index and middle fingers placed externally at the mandibular angle and the index of the other hand placed intraorally at the medial side of the mandibular angle.
External Pterygoid: for the superior head palpation is extraoral with the middle finger placed below the zygomatic arch about 2 cm anterior to the tragus, asking the patient to open the mouth to reveal the superior concavity of the mandibular notch. For the inferior head, palpation is intraoral placing the little finger between the upper and lower arch causing the mandible to deviate ipsilaterally to move the coronoid process outward and allow fingers to insert into the fornix between tuber and coronoid to gently reach the most medial posterosuperior area possible.
The trapezius and sternocleidomastoid muscles, although not directly responsible for masticatory movements, are examined given their close relation to the position of the temporomandibular joint and head.
Sternocleidomastoid: palpation is performed bilaterally starting from the mastoid insertion behind the ear sliding fingers along the whole muscle length to its insertion at the middle third of the superior face of the clavicle and the anterosuperior face of the manubrium sterni. The exam can also be done by pinching the muscle belly along its entire length.
Trapezius: palpation is performed at its origin at occipital level and cervicodorsal spine and insertion at the lateral third of the clavicle, scapular spine and acromion sliding fingers along its entire muscular body or pinching gently between thumb and index finger.

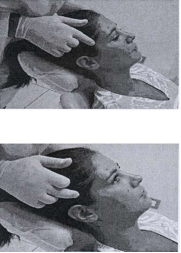
5.3.2.2 Joints
Both joints must be analyzed with palpation to assess the presence of asymmetric movements and sensitivity during the maneuver. Moderate pressure is applied in maximal intercuspation and during lateral, opening, closing, and protrusive movements. The maneuver is performed analyzing laterally and posteriorly separately, palpating both TMJs simultaneously so the patient can report any difference in pain sensation and the operator can assess any asymmetric movement or intra-articular impediments.
Lateral palpation: performed by placing the index and middle fingers on the lateral pole of the condyles just anterior to the auricular area. If this evokes pain, it suggests involvement of the articular capsule or lateral pterygoid muscle.
Posterior palpation: performed by exerting gentle anterior pressure with the little finger inserted into the external auditory canal. Pain evocation suggests involvement of articular or retroarticular soft tissues.
TESTS:
JOINT PLAY : this maneuver separates, within limits, the condyle-disc complex from the temporal component by forced mobilization of the joint in the three spatial planes. It must be done gently without evoking pain to avoid muscle elevator reflex contraction; the mandible must be as relaxed as possible, and the head well supported and fixed against the examiner’s body. Joint play is evaluated by distraction and translation to assess soft tissue elasticity (ligaments and capsule) and any intra-articular alterations. The operator stands behind the patient, blocking the head against their chest and placing the thumb on premolars and molars on the test side, supporting the mandible with the rest of the hand. Palpation of the joint is done with the middle finger of the hand blocking the head while exerting downward or forward-medial pressure intraorally with the thumb.
JOINT/MUSCLE TEST: maneuver used to highlight any pain presence during joint movements in physiological planes. The operator stands behind the patient, blocking the head against their chest, placing palms of both hands against the chin. The patient is asked to perform different movements to examine various muscle groups. Pressure is first exerted to oppose but not block movements, then increased to strongly oppose until movements are blocked. Each test lasts about 30 seconds.
- AUSCULTATION
Joint noises such as clicks and crepitus are detected by palpation and auscultation. Attention must be paid since the mandible is a single bone, so noise generated in one joint always propagates to the other.
- ARTICULAR RANGE OF MOTION
Assessment of joint mobility provides useful information on range and quality of motion and presence of pain during execution.
Active opening: measurement of maximal mouth opening using calipers or ruler referencing upper incisor margin and ideal overbite line of upper incisors over lower. Normally, values range from 40 to 55 mm. Mandibular path deviations in the frontal plane should also be observed as they may indicate joint, disc, or muscular problems. Opening under this range is considered reduced; in cases of constitutional ligament laxity, values over 55 mm occur. Limitation due to intracapsular alterations occurs between 20 and 30 mm. Muscular problems can cause limitation at any point, but limitation around 8-10 mm is almost certainly muscular in origin.
Passive opening: after patient actively opens maximally, the operator places thumb on upper incisor margin and index on lower incisors, gently forcing to increase interincisal distance without pain. Elasticity and rigidity sensations and opening increase (usually 2-3 mm) are evaluated. Values over 2 mm suggest muscular origin of dysfunction. Conversely, if opening cannot be increased and feels "rigid," a mechanical intracapsular block is suspected.
Active lateral excursion: measurement of mandibular displacement during maximal lateral movement right and left. Amplitude is symmetrical and usually between 8 and 12 mm.
Passive lateral excursion: achieved by forcing maximal active lateral excursion. Endfeel and increase of motion amplitude (usually 1-2 mm) are evaluated.
Protrusion: movement magnitude is obtained by adding overjet value to distance between upper incisor surfaces and lower incisor incisal edge after maximal protrusion. Normal range is 10 to 12 mm with straight movement.
- POSTURAL EXAMINATION
Morphological exam and Barré vertical study
Variations of main landmarks are sought in the three planes (frontal, sagittal, horizontal) relative to an ideal orthostatic position model with special reference to skull, spine, pelvis, and lower limbs. Asymmetries and rotations of skeletal segments as well as areas of altered trophism and/or muscle tone are also evaluated.
“SCANPOSTURE” SYSTEM
Acronym of scan an analysis of postural relation, this system is a methodical approach to analyzing variations generated by introducing variables in postural inputs.
It is a postural exam mainly aimed at the three primary postural inputs: eyes, mouth, and feet. Particular attention is paid to simultaneous acquisition of the three data in the three spatial planes.
The system, highly customizable and based on an integrated visual and instrumental approach, significantly differs from scolioscope analyses, Barré vertical (French standardization), and stabilometric platform analyses, due to principles and methods used.
The possibility to evaluate interconnections between the stomatognathic system and other systems is mediated by a consequential differential approach. Once a “baseline” (habitual postural attitude) is acquired, ad hoc variables are introduced, e.g., first the eyes-closed test which may reveal ocular torticollis, then an occlusal release test which may reveal occlusal torticollis.
ANALYSIS TOOL
To more effectively investigate variations and avoid false positives as much as possible, the Barré vertical methodology has been modified. Firstly, French normalization indicates a view from behind, as the technique was designed to appreciate body parts such as spine, scapulae, hips, and intergluteal line. No importance is given to gaze attitude or instant occlusal situation. Lateral projections are obtained by rotating the patient 90° causing a new postural attitude. Since analysis cannot be performed in a totally uniform 360° space, gaze will inevitably fix on elements not necessarily at the same height or distance and often not aligned with the vertical, resulting in discrepancy between four photos (rear, right side, left side, front).
The Scanposture system is based on six essential bases:
- Do not move the patient and acquire data simultaneously.
- Analyze the patient facing a precise target in front of them.
- Perform profile analysis simultaneously with frontal analysis.
- Require an unchangeable station to compare acquisitions over time.
- Perform digital photographic acquisitions.
- Have simultaneous podalic integration (podoscope, scales, stabilometric/baropodometric platform).
All this is achieved by a small modification of the scolioscope concept. Starting from the assumption that a plumb line in front of the patient can unconsciously induce realignment or shift towards the dominant eye side, the plumb line and symmetry lines in front of the patient were removed. A squared backdrop and a perfectly aligned median line with a rigidly fixed digital camera on the opposite wall were created. This eliminates the need for plumb lines and prevents parallax effects. To simultaneously acquire front and profile images, a lateral mirror was added. A baropodometric platform under the feet provides immediate and understandable information.
ACQUISITION FORM
Habitual
This term indicates the patient's “status,” including any glasses or contact lenses, without any reference or attention to current occlusal position. In practice, no information is given; the patient is instructed to fixate a predetermined point and stay relaxed, not at attention as usually.
Short leg or hump
The patient, standing with feet together aligned to symmetry lines in front of the platform, is asked to bend at 90°. A smooth movement is requested, first bending the head then the trunk, without bending knees and keeping arms extended. The desired position is held and a photo is taken. Normally, a hump is generated on the short leg side.
Habitual feet together
The feet together test is a stress test but with high repeatability over time. It is the only always identical and repeatable position allowing analysis of postural system evolution during therapy.
Patient’s comfortable position with feet symmetric relative to the median in habitual and with any glasses
This is the true start of acquisition for differential diagnosis. Actually, this acquisition is not exactly repeatable because foot position can vary between days. It is considered a “baseline” because it captures the “normal” objective situation of the patient and their postural evolution over time. Evolution includes changes in plantar support patterns. Often flat or high feet normalize due to unconscious reduction of extra- or intra-rotation of a foot.
Variance test without glasses
If glasses are present, this test analyzes possible changes in head position.
Variance test with glasses
This test confirms the importance of the visual system and gives information about what would happen if glasses were removed.
Test with occlusal splint (optional)
Allows verification of dental occlusion’s influence on posture.




