Biomechanics of the Relationship Between the Temporomandibular Joint and Posture
Dr. Mauro Lastrico
Temporomandibular joint and posture relationship
Dr. Ft Mauro Lastrico
excerpt from:
Dr. Mauro Lastrico
Musculoskeletal Biomechanics and Mézières Method
Marrapese Editions
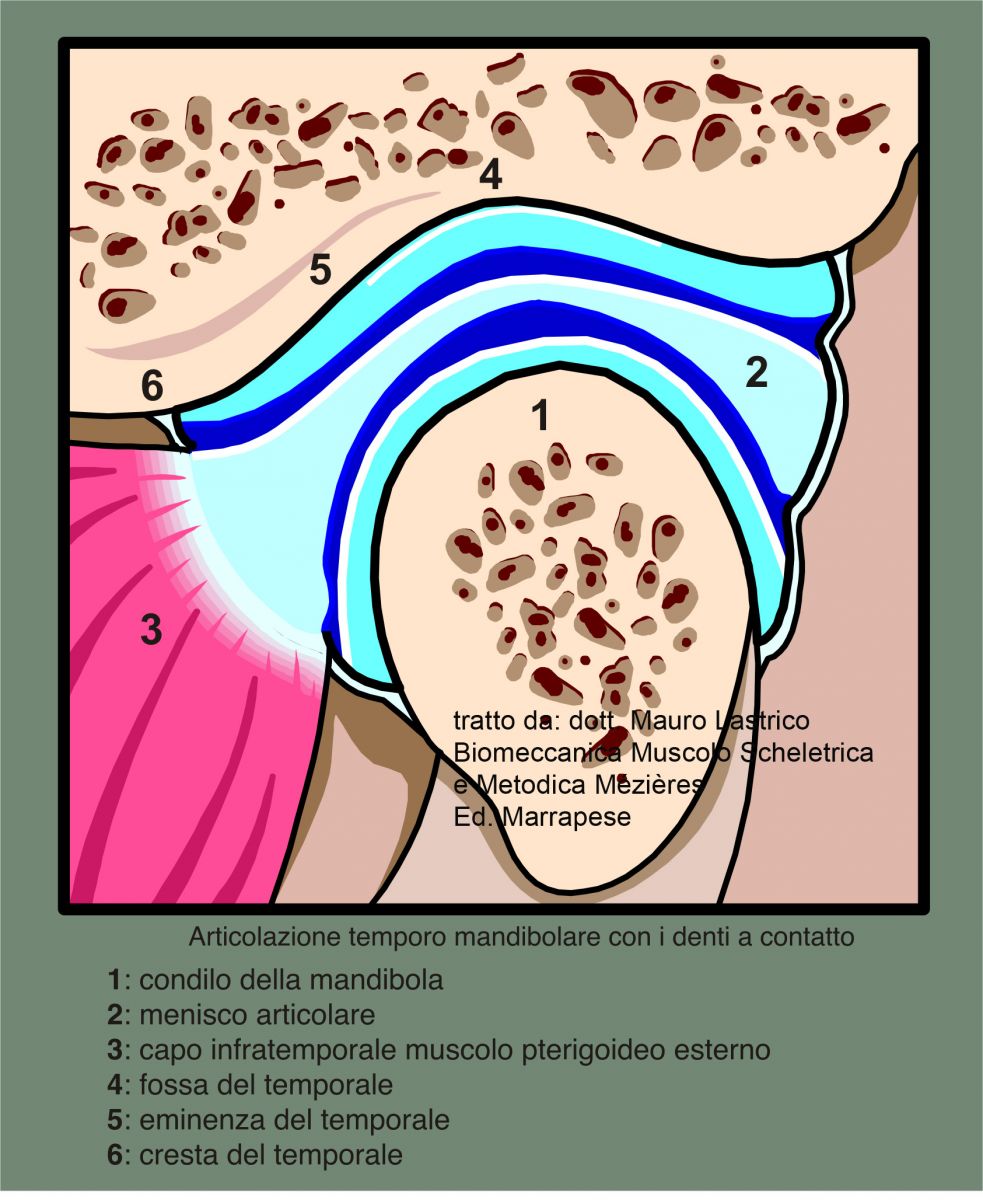
The TMJ is actually a double convex-concave and concave-convex joint between the mandibular condyle, the meniscus (which has an articular function), and the temporal bone.
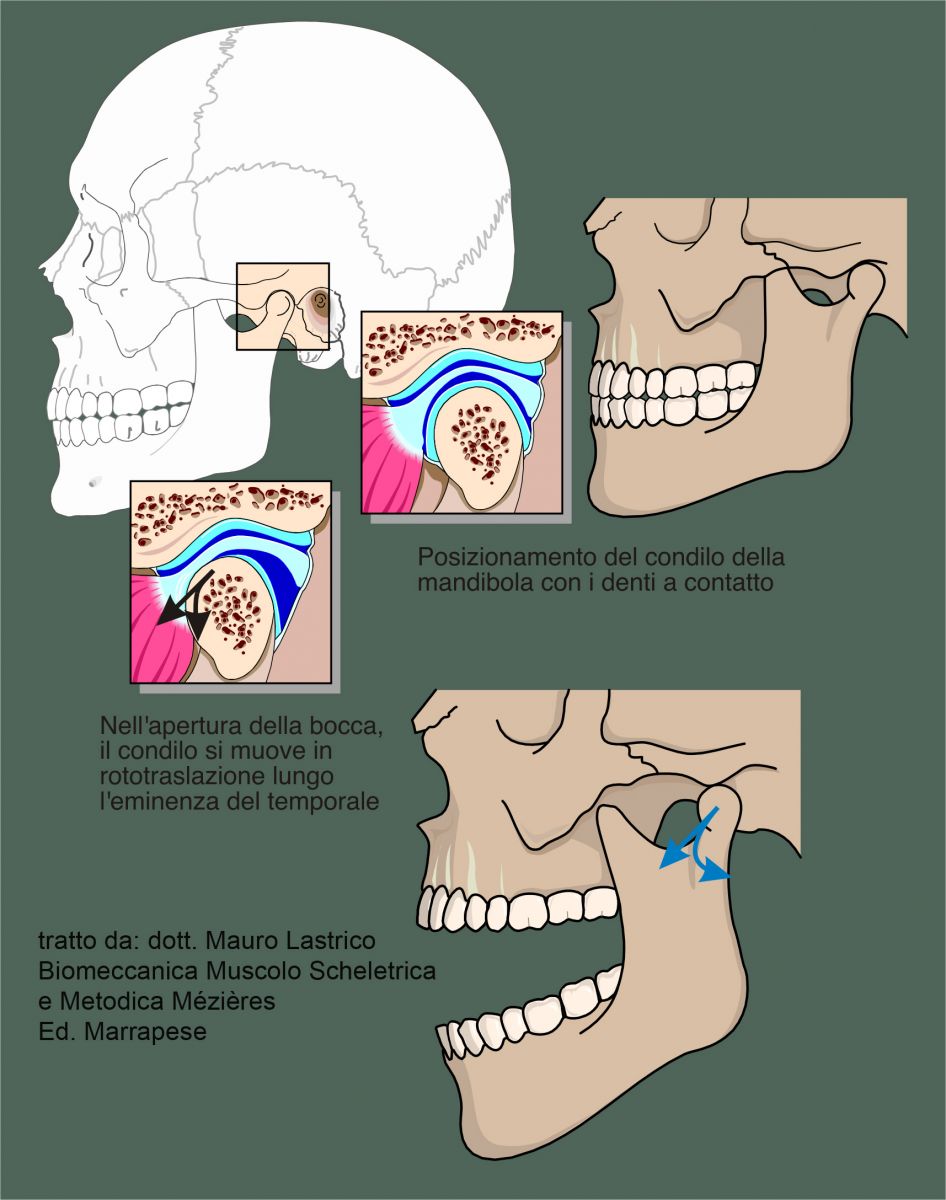
With the teeth in contact, the physiological position of the condyle is not inside the temporal fossa but along the straight path (temporal eminence).
During mouth opening, the mandibular condyle moves along the eminence through a rotary movement opposite to the movement's direction (otherwise the mandible would close).
The muscles acting on the joint are: masseters, temporals, and internal pterygoids which act as a lock; external pterygoids control positioning movements of the mandible and lateral movements; suprahyoids and infrahyoids open the mandible.
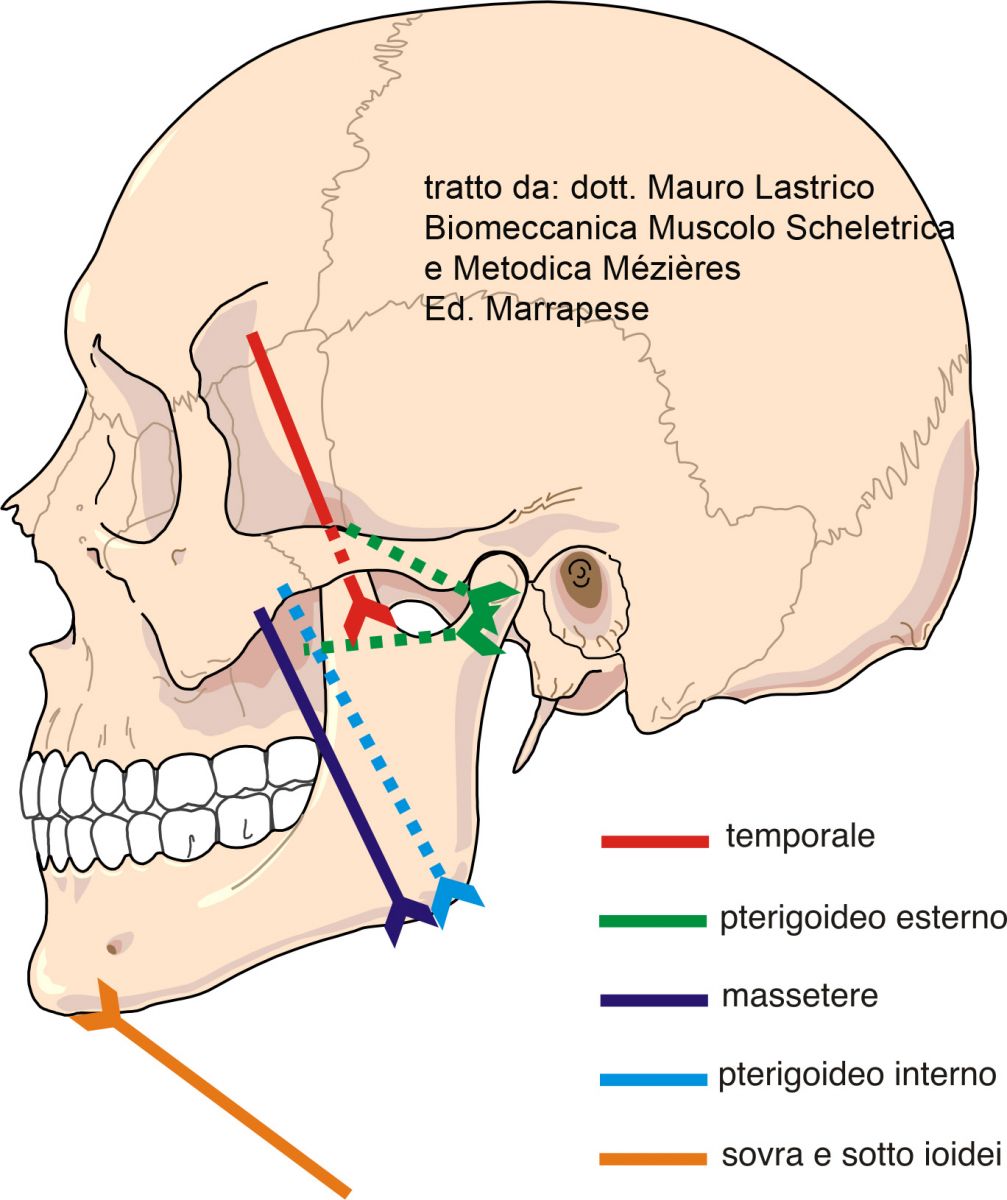
These muscles, although monoarticular, can interact with other muscles due to the characteristics of complex systems.
The connection between problems related to the masticatory muscles and various body districts passes through the hyoid bone, which is muscularly connected to the cervical vertebrae and scapulae.
Physiology of swallowing.
Swallowing is an involuntary movement that occurs several times per minute. To allow it, the masticatory muscles contract bringing the teeth into contact.
If the dentition is correctly and physiologically positioned, the masticatory muscles act with equal intensity using the minimum necessary force. The locking of the teeth will occur so as not to influence other body districts, that is physiologically. Therefore, no correlation between occlusion and posture will be determined.
Connection between occlusion and posture
Physiologically, there should be no connection between dental occlusion and posture: however, if the dentition is pathologically positioned, this connection can occur.
The way in which even a slight occlusal imbalance can affect the body's posture is nonlinear.
While in linear mathematics there is a direct proportion between stimulus and effect, in nonlinear mathematics even a small change can produce significant effects.
From a linear point of view, therefore, occlusal imbalances should not cause large displacements of body masses, which is instead possible from a nonlinear point of view.
Being a nonlinear relationship, not all people with occlusal problems will have altered postural patterns.
The most commonly found events are three:
- difference in tooth length (pre-contact)
- excessive free space
- decrease or absence of free space
Difference in tooth length (pre-contact)
In cases where a dental arch has teeth that are too short or too long, during mouth closing movements the masticatory muscles act asymmetrically (right-left) and with intensity greater than physiologically necessary.
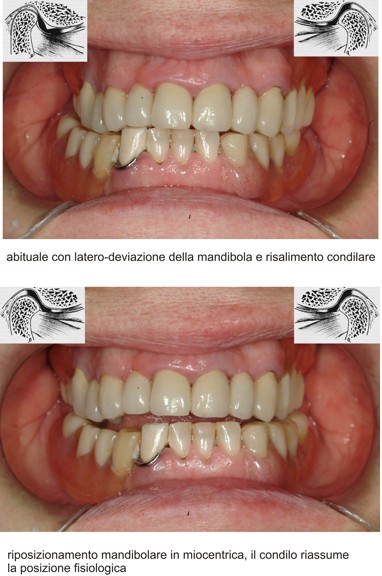
The first consequence will be that the mandibular condyle on the "short" tooth side, to allow contact, will have to position itself beyond the physiological position, towards the temporal fossa. The mandible will thus have a torsional movement.
Since there are many receptors inside the mandibular fossa, this event can trigger painful symptoms mostly localized in the TMJ, ear, and head.

The image shows a crossbite with lateral deviation of the mandible. On the right (patient's side), the pathological dental contact causes the mandibular condyle to rise with anterior projection of the articular disc.
Furthermore, asymmetric and excessive muscle activation will involve other muscle districts through the action of the hyoid muscles.
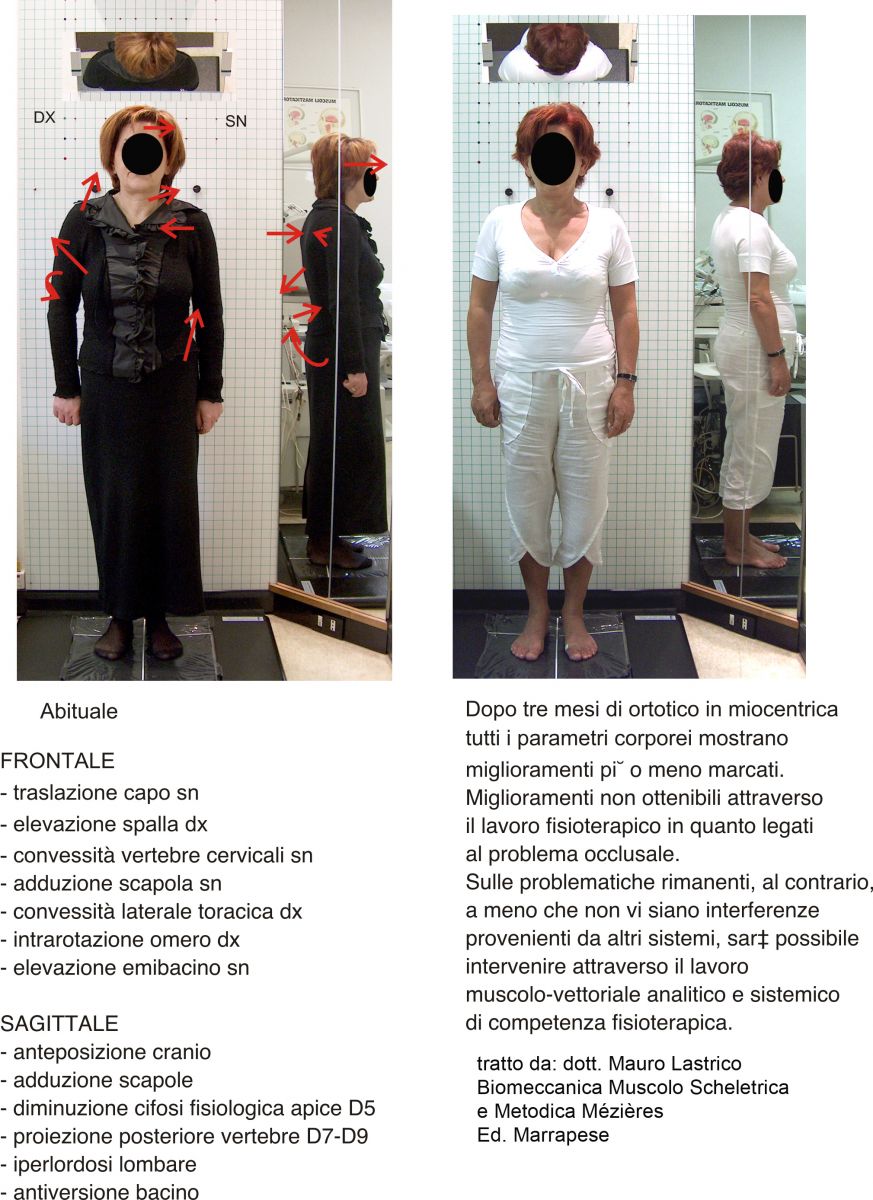
Excessive muscle intensity or tension will therefore not be limited to the masticatory muscles only and other joints will suffer the consequences of the pulling muscle forces. The cervical vertebrae will lose their symmetrical position and one shoulder may be elevated.
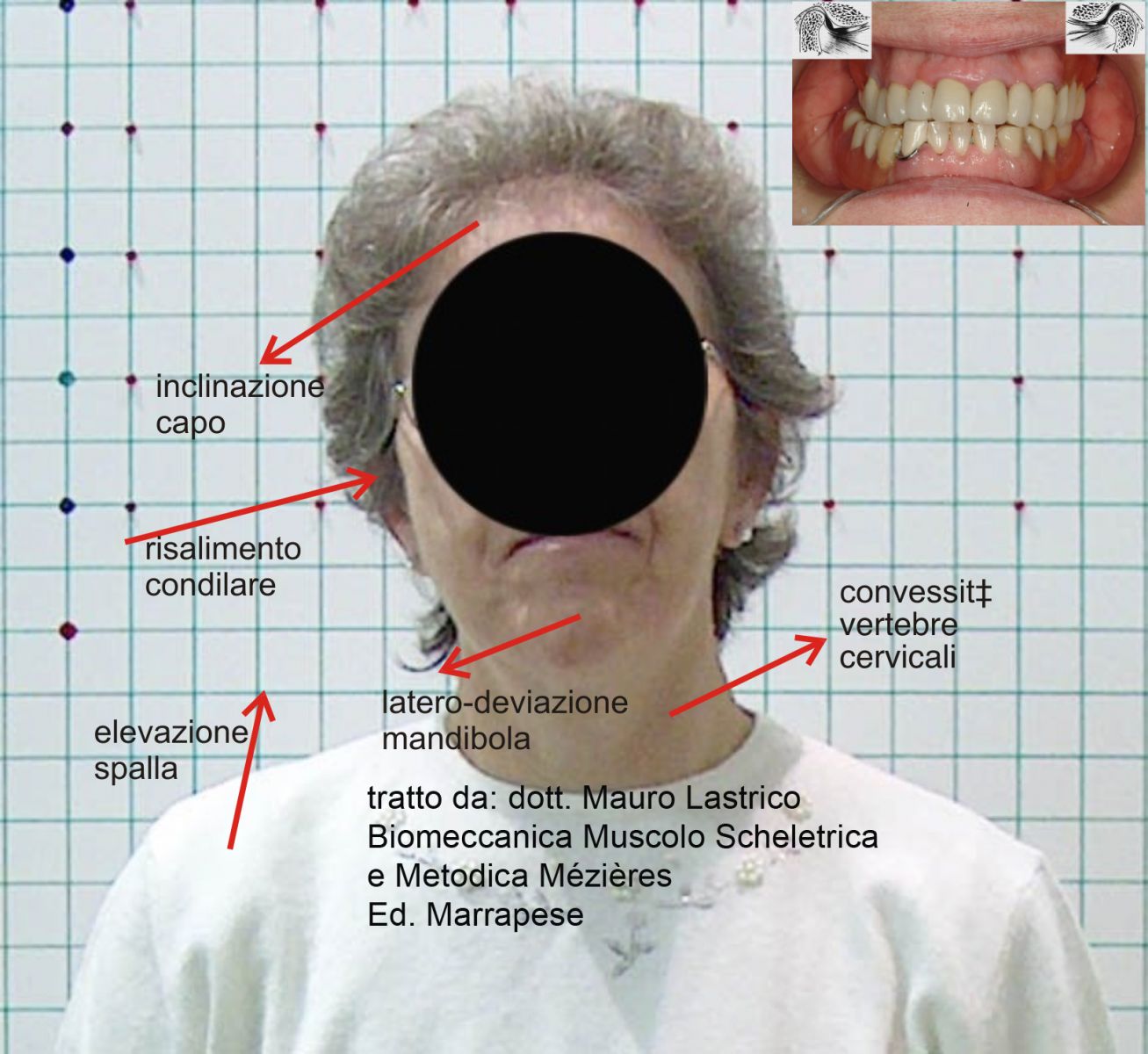
and, if the process lasts over time, a complex series of skeletal alterations may occur. That is, there will be an alteration of body posture.
Excessive free space
At rest, that is with relaxed masticatory muscles, the posterior teeth should not be in contact but present a "free space" of about 2 millimeters. This is the condition considered rest and physiological by the brain centers.
If the free space is excessive, for example due to generally "too short" teeth, to maintain a correct free space the masticatory muscles would have to be permanently tense. To compensate for this continuous effort, the muscular system and in particular the muscles in front of the cervical spine, taking a fixed point on the third thoracic vertebra, move the entire head forward, acting synergistically with the scalenes.
This way, the dental arches get closer, unloading the work of the masticatory muscles.
However, moving the head forward also means shifting the body's center of gravity.
To avoid losing balance, the underlying muscle districts will have to activate modifying the entire vertebral sinusoidal curve, consequently changing the verticality of body segments.
Again, this will result in a postural alteration.
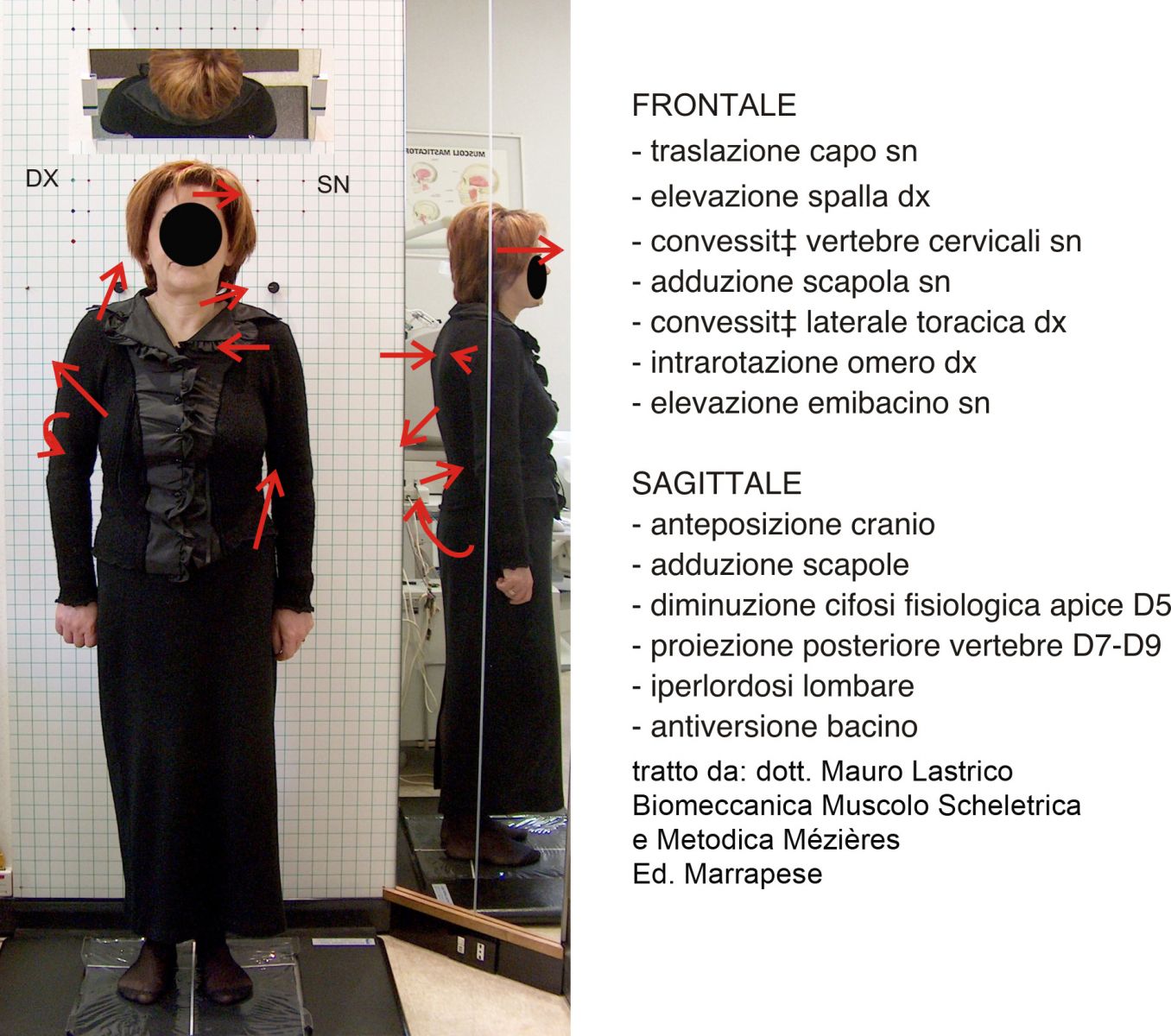
The above photo shows the anterior projection of the head and systemic postural alterations caused by decreased tooth height (images below)


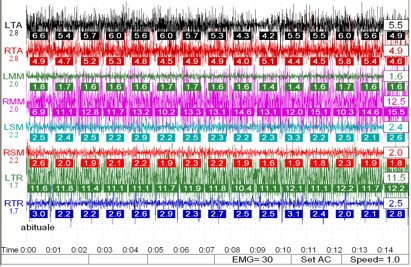
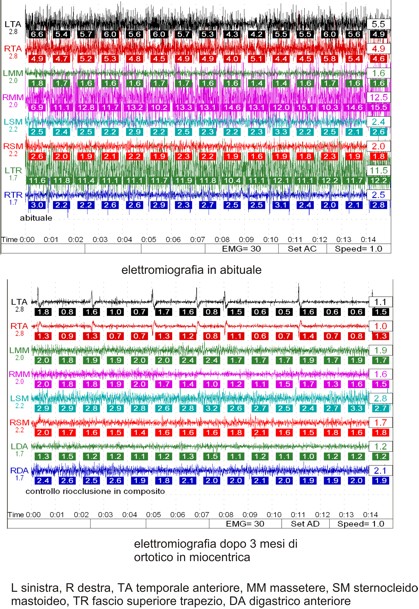
The resting electromyographic tracing of muscles shows hyperactivity and right-left asymmetry: L left, R right, TA anterior temporal, MM masseter, SM sternocleidomastoid, TR upper trapezius bundle.
Decrease or absence of free space
It is the opposite problem to the one seen before._In this case the muscles behind the cervical spine will activate to move the head backward. In this way, the dental arches separate unloading the work of the hyoid muscles.
Again, the body's center of gravity will shift, this time posteriorly, and again the underlying muscles will have to activate to maintain balance, acting on the entire spine and altering the verticality of body segments.
The consequence will be a postural alteration.
All the postural imbalances seen may in turn generate the onset of orthopedic pathologies (scoliosis, low back pain, cervical pain, etc.) which could be defined as secondary to a primary pathological involvement of the stomatognathic apparatus.
Connection between posture and occlusion
The analyzed mechanisms can also act in reverse, that is, it could happen that a muscular imbalance from other body districts determines, due to muscular interconnection mechanisms, occlusal problems generating condylo-menisco-temporal conflicts.
The muscular apparatus as a complex system can undergo primary (intrinsic to the system) or secondary (caused by malfunction of other structures) shortenings. In both cases, a postural problem will manifest over time.
Diagnosis
Temporomandibular joint dysfunction is never a cause (except rheumatoid arthritis and articular rheumatism), but a consequence of other problems for which, more correctly, cranio-cervico-mandibular disorders (CCMD) will be discussed.
These disorders can have a stomatognathic or extrastomatognathic starting circuit:
stomatognathic origin, that is dental, circuit: bad skeletal mandibular-cranial relationship > muscle tension > mandibular deviation > joint compression > TMJ problems;
extrastomatognathic origin, circuit: any alteration of head posture induced by biomechanical problems or other systems (visual, auditory, etc) > muscle tension acting on the mandible > mandibular position change > joint compression > TMJ problems.
Cranio-cervico-mandibular disorders of stomatognathic origin often cause systemic postural imbalances.
Collaboration with a dentist-gnathologist is necessary both in performing differential diagnostic tests and subsequently in setting the most appropriate therapeutic path.
Some symptoms may indicate skeletal-postural problems deriving from the stomatognathic circuit with consequent TMJ problems:
- ear pain (in the absence of ENT problems)
- joint noises and difficulty opening and/or closing the mouth
- headache
- cervicobrachialgia (with forward or backward head posture)
- low back and/or dorsal pain (with forward or backward head posture)
Clinical tests
Some clinical tests can reveal dysfunction of the temporo-menisco-mandibular joint:
- the operator places the pinky finger in the patient's ear canal with the mouth open. Asking for mouth closing, he can feel if there is a rise of the mandibular condyle in the temporal fossa. Under physiological conditions, with teeth in occlusion, the operator's finger should not feel contact with the mandibular condyle
- the operator, placing hands outside the joint, asks the patient to open the mouth detecting possible subluxations or endo-articular noises
- the operator manually contacts the patient's temporal and masseter muscles and asks them to rhythmically clench the mandible. Observation aims to detect simultaneity and equal muscle contraction intensity
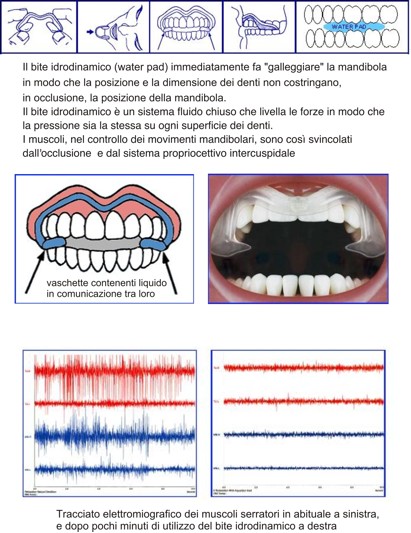
- observe postural variations using a hydraulic bite with communicating vessels, that is a hydrodynamic bite. This type of bite, preventing the patient's habitual dental occlusion, reprograms mandibular movement into muscular equilibrium (reprogramming occurs at each swallowing). If the position of the teeth interferes with posture, sensitive variations in body posture, cervical vertebrae realignment, and hyoid bone repositioning will be observed. Subjectively, the patient may report sensations of well-being in the cranio-cervical area and also in the underlying body districts. The hydrodynamic bite is used during examination and is not a therapeutic means.
If these tests are positive, in a causal logic, referral to a gnathologist becomes advisable.
Treatment
If differential diagnosis shows a postural problem deriving from a stomatognathic origin, the first intervention must be from the dentist using a bite or orthotic. These (removable) devices, preferably placed on the lower dental arch, aim to achieve correct dental contact for proper swallowing and, consequently, a physiological temporomandibular joint positioning.
Later, when the system has stabilized, the opportunity to act permanently on the teeth will be evaluated.
Between bite and orthotic, the latter is preferred for its precision and its characteristic, being intercuspidated, of reproducing the optimal dental position. To use this device, the dentist-gnathologist must use the kinesiograph, a complex tool that allows modeling the orthotic respecting physiological lines; the goal is that intercuspation during swallowing occurs not only with the mandibular condyle in physiological position but also balanced muscle forces.


Conclusions
Discussing the interference of the stomatognathic apparatus on posture, it was highlighted how systemic muscle shortening is secondary to a primary structural problem.
This problem occurs quite frequently. In the author's personal case history, about 30% of cervicobrachialgia symptoms are supported by occlusal problems; the percentage is lower (but not zero) for those involving underlying body districts.




