Biomechanics of Ideal Posture
Dr. Mauro Lastrico
Biomechanical model:
the ideal posture
Dr. Mauro Lastrico, physiotherapist.
Extracted from:
"Musculoskeletal Biomechanics and Mézières Method"
Author: Dr. Mauro Lastrico
Marrapese Publisher
In the evaluation of both static and dynamic postural alterations, reference will be made to an "ideal biotype." This biotype is extrapolated through an "engineering" type model. A reference model, that is, which refers to the best possible biomechanical solution concerning physiological joint sequences.
Ideal posture
Every part of the body has its own center of gravity; the body's center of gravity is the resultant sum of each of these.
The projection to the ground of the human center of gravity in an upright stance is the ideal vertical line that falls at the center of the area delimited by the foot support surface.
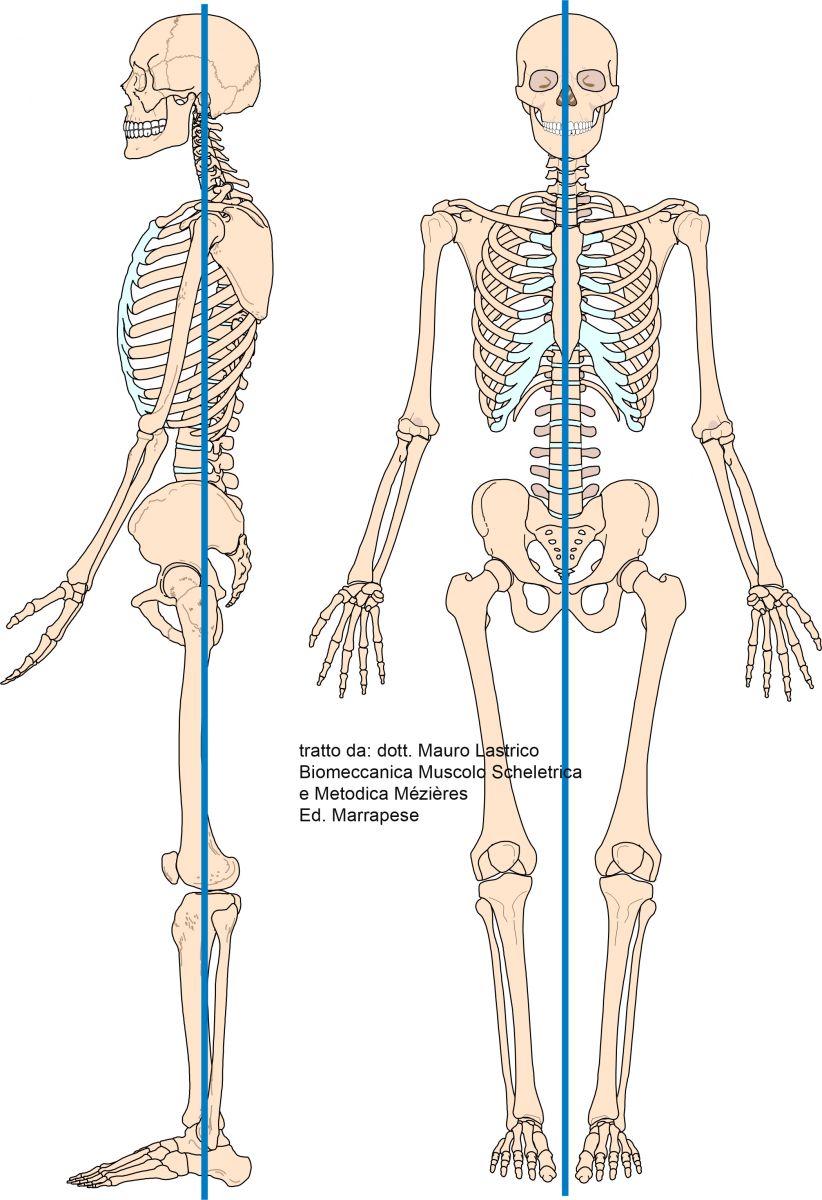
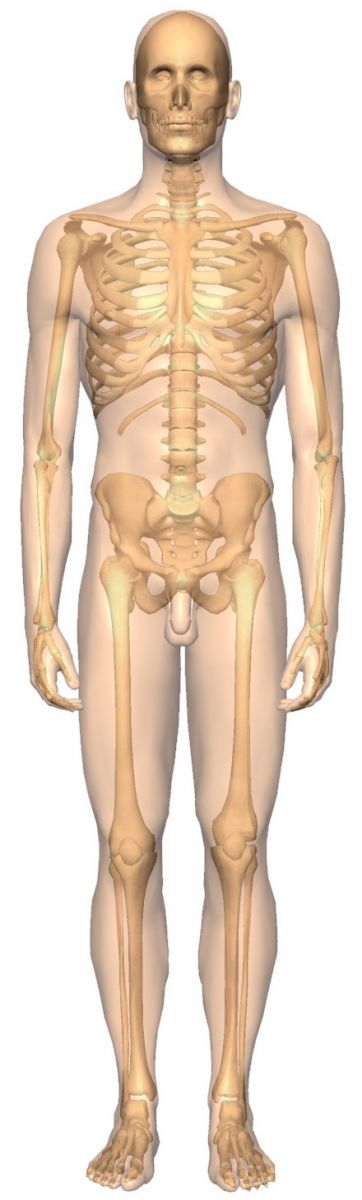
From a biomechanical point of view, in the body's ideal symmetrical side posture, the vertical projection of the center of gravity (or resultant barycenter) passes:
* anteriorly to the lateral malleolus
* anteriorly to the knee joint
* posteriorly to the hip joint
* through most of the lumbar vertebrae
* through the acromioclavicular joint
* through the cervical vertebrae
* through the external auditory meatus
When observed from the front or back, the body appears divided into two perfectly symmetrical parts and the vertical projection of the center of gravity passes through the malleolar center.
Specific static parameters
In static observations, the patient will be observed frontally, posteriorly, and laterally. The constant constraint will be the position of the feet, which, if possible, should have heel and first metatarsal in contact, and the gaze oriented forward. This is to allow the reproducibility of the observation and to exacerbate adaptations. Also statically, observation will be performed in a supine position on the ground.
Frontal observation
The following is a list of the main parameters; any other observable element will prove useful in functional evaluation.
The big toes should be in contact along their entire length and free of rotations;
The toes at rest should be free of flexions, rotations, lateral deviations and should not participate in maintaining the upright stance;
The lower limbs should have four points of contact:
* malleoli
* calves at the upper third
* medial femoral condyles
* thighs at the upper third
Frontal observation at the knees will observe the position of the patellae;
Of the pelvis, three parameters will be recorded:
* translation
* elevation
* rotation
Of the shoulder girdle, two parameters:
* lateral thoracic convexity
* rotation
The waist triangles will be observed, consisting of a base described by the profile of the upper limb up to the contact with the hip joint and two legs described by the lateral thoracic border and that of the quadratus lumborum muscle; the two legs should not show acute angles;
Of the shoulders, two parameters:
* elevation
* anteposition
Of the clavicles, two parameters:
* trend relative to the horizontal (ascending or descending)
* apparent length difference
Of the upper limbs, four parameters:
* humeral rotation (the intercondylar line should be perpendicular to the body's median line)
* elbow
* forearm position
* hand position
Of the skull, two parameters:
* inclination
* rotation
The eye fissure
Any lateral deviation of the mandible.

In the above image, the axial skeletal alterations of two patients.
Besides the differences between the two hemibodies, the individual barycenters are not aligned with the line passing through the malleoli. Muscle tone will therefore have to increase to allow the maintenance of the upright stance.
Posterior observation
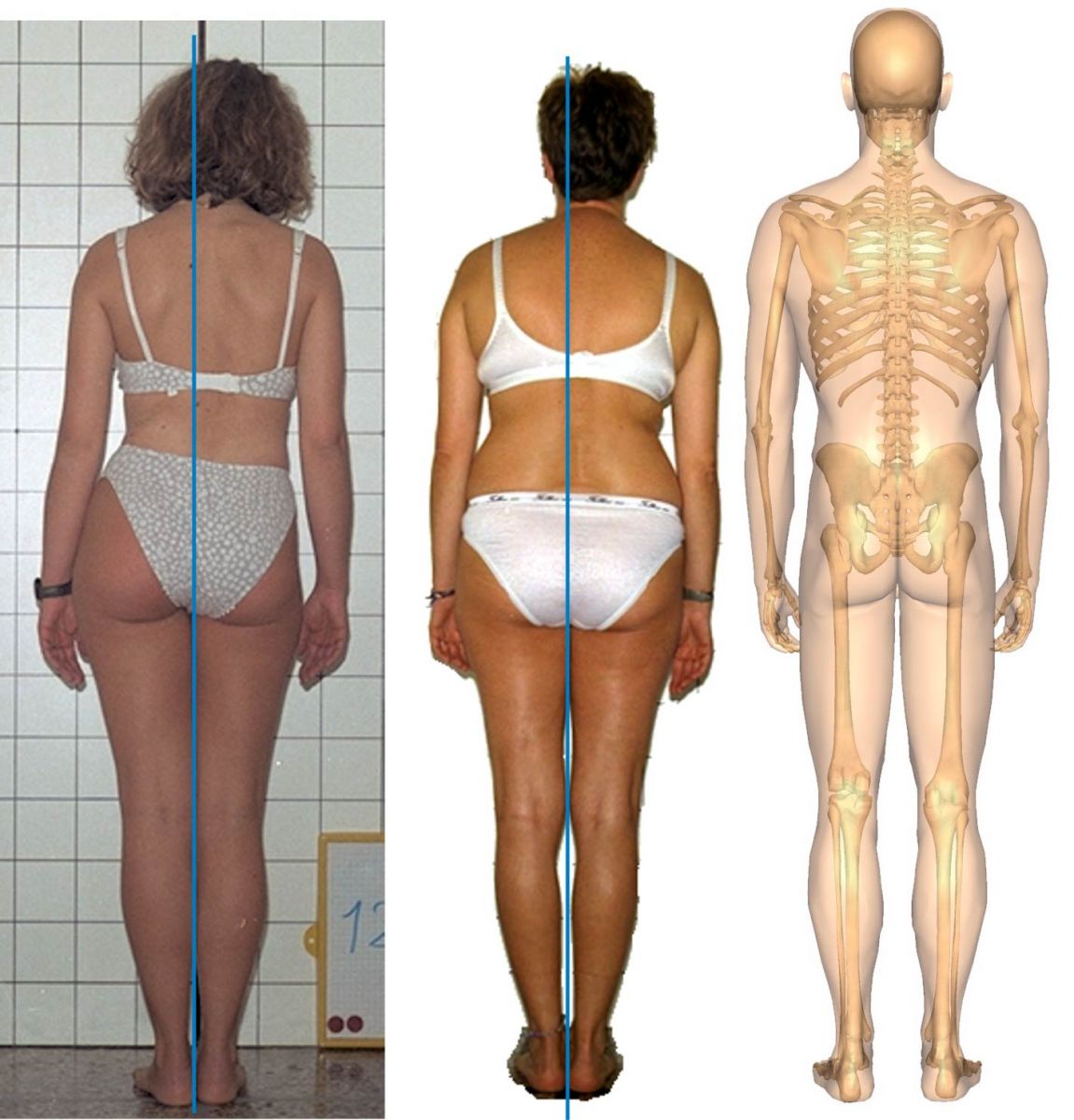
Besides verifying the data collected frontally, further specific observations will be made posteriorly.
The Achilles tendons should be parallel and vertical
The knees will be evaluated for:
* femur rotation (the four femoral condyles should be on the same line perpendicular to the median line)
* presence of flexion or recurvatum
The gluteal lines, which should be present, deep, and long.
Manually and visually, the vertebral sinusoid will be checked, noting abnormal trends in both sagittal and frontal planes;
The relationship between the medial scapular margins and the D5 spinous process, which should be on the same line;
The reciprocal relationship between the scapulae
Lateral observation
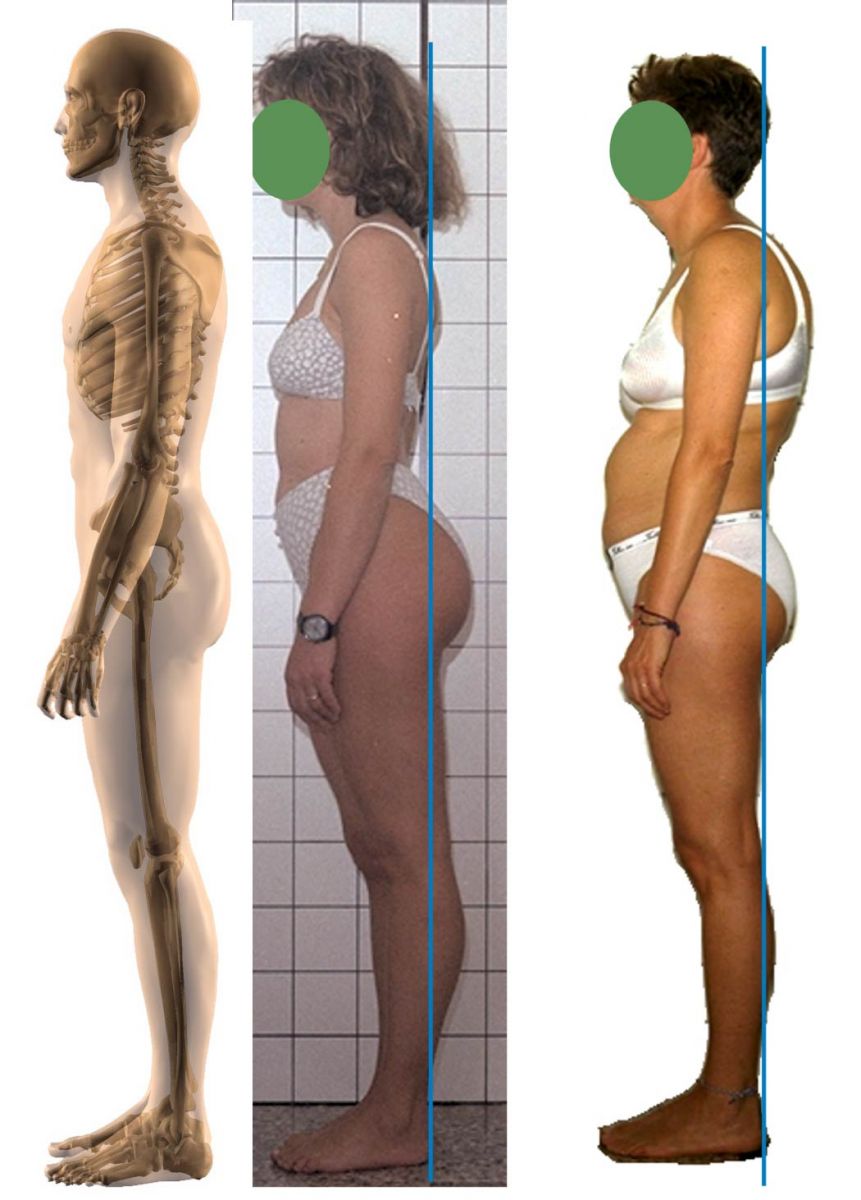
Again, the observational plane will be used, both to check some previous data and to evaluate new ones.
The insertion tendon of the peroneals should pass behind the lateral malleolus.
Compared to an ideal line intersecting the Achilles tendons and perpendicular to the ground, four contact points should be found superiorly:
* upper third of the calf
* glutes
* D5 vertebra
* occiput
The sternal line should have an inclination of about 30 degrees relative to the vertical passing through the sternal manubrium.
The imaginary line drawn between the xiphoid process and the pubis should be straight and vertical.
The pelvis should be neither anteverted nor retroverted.
Supine observation on the ground
It will occur in two steps: initially asking the patient to position themselves as they feel upright. This will provide information about their body schema, that is, whether there is correspondence between their subjective sense of upright and reality. Subsequently, they will be passively aligned considering the malleolar center, pubic symphysis, jugular notch of the sternal manubrium, and skull.
In the supine clinostatic position, no muscle is forced to activate to maintain the position. Consequently, this type of exam will be the most relevant as it will provide information on which muscles are effectively shortened and on inevitable skeletal alterations.
In contrast, in the upright stance, all asymmetries provide information about the muscular strategies involved to maintain it.
Observations will concern both the sagittal and frontal planes and will include all the elements previously seen, noting that often many data from previous projections are reversed.
Added will be:
* palpation of the cervical and thoracic vertebrae up to D3, to verify any vertebral rotations or translations (up to D3, because below this level thoracic vertebrae are interdependent with the thorax);
* palpation of the temporomandibular joint to assess any rises of the mandibular condyle in the temporal bone fossa or condylar subluxations;
* palpation of the lumbar vertebrae;
Dynamic observations
Dynamic observations will concern both active movements performed by the patient and passive movements performed by the operator.
Active dynamic observations aim to detect whether the actions performed by the patient are carried out by anatomically designated muscles or whether substitute moments (emerging abilities) are present.
Passive dynamic observations aim to detect abnormal musculoskeletal relationships.
The reference in both cases is the theoretical anatomical model.
Primary and secondary muscle shortenings
Posture is the multifactorial resultant of elements coming from many systems: vestibular, masticatory, skeletal, muscular, visceral, visual, emotional, fascial, etc., that is, from the integration of neurophysiological, psychosomatic, and biomechanical mechanisms.
Every structural alteration coming from a single system will cause adaptations that will manifest both with a local alteration in the district of origin and systemically.
Micro alterations may be present without causing significant adaptations, and it is therefore necessary to identify the dominant factors, using postural tests and collaborating with individual professional specialists in their own field of interest.
The way a district alteration becomes systemic is determined by muscular connections: a limb with length discrepancy adapts mechanically with adjacent structures but, through the muscular system, the problem reverberates on the entire body. Any physiotherapy treatment aimed at rebalancing the muscular forces acting can only be transitory if the means suitable for solving the original problem, i.e., the length discrepancy, are not intervened upon.
Wishing to act with a causal logic in treating postural changes, the initial investigation must differentiate the primary or secondary origin of muscle involvement.
In the first case the treatment is mainly physiotherapy, in the second case physiotherapy treatment is subordinated to the therapeutic action aimed at the dysfunctional apparatus of origin.
Copyright © 2025 AIFiMM Formazione Mézières Provider E.C.M. n. 1701. All rights reserved.



