Systemic and Segmental MSK Biomechanics – Online Course
Physics-based assessment and treatment of musculoskeletal pathologies
An advanced online course designed for physiotherapists and rehabilitation professionals seeking a structured clinical reasoning model for chronic musculoskeletal dysfunctions, recurrent or resistant to conventional treatments.
| Course format and certifications • On-demand online course (self-paced) • 18 video modules — 32 hours • Downloadable PDF materials — approx. 6 hours • Total learning time: 38 hours • Certifications: 38 CPD hours (UK) · 45 contact hours / 4.5 CEU (Florida, USA) |
The biomechanical framework taught in this course is built around three core clinical questions:
-
WHY a joint or spinal segment is mechanically altered
-
WHEN the symptom is local or the expression of a referred or systemic organization
-
HOW to intervene both at the segmental and systemic level
Vector-based biomechanical analysis is the tool that makes this interpretation possible.
It allows clinicians to move from observation to prediction, and from prediction to targeted intervention.
This is applied physics in daily clinical reasoning
This model is particularly effective for:
-
Chronic musculoskeletal symptoms unresponsive to conventional treatments
-
Pain that alternates or migrates between body regions
-
Recurrent issues without clear traumatic cause
-
Persistent functional limitations post-surgery
-
Orthopedic pathologies
Expected Treatment Timeline
The timelines below are clinical estimates and may vary depending on diagnosis, comorbidities, and whether the dysfunction is primary or compensatory.
Symptomatic improvement: In primary muscular dysfunctions, measurable changes in joint alignment and symptom reduction typically appear within 2–10 sessions (approximately 60-minute sessions at weekly frequency), depending on clinical presentation severity and accuracy in identifying causal vectors.
Long-term stability depends on the depth of systemic rebalancing achieved. Clinical experience from clinicians using this approach indicates that more extensive treatment courses tend to produce more stable results over time.
Some patients choose to discontinue treatment after symptomatic remission, still obtaining short- to medium-term benefit. Continuing beyond the symptomatic phase consolidates vector rebalancing and reduces recurrence probability.
Treatment non-responders: As in all clinical practise, approximately 10–15% of patients may show limited or meanigful response to treatment. This percentage reflects normal biological variability, complexity of the therapeutic relationship, and cases in which the primary cause lies outside the domain of muscular biomechanics.
Persistence of symptoms beyond 10 sessions requires systematic reassessment: initially unidentified compensations, accuracy of vector analysis, or the presence of non-muscular primary causes requiring a multidisciplinary approach.
A recurring phenomenon is observed in clinical practice: muscles tend to progressively shorten over time. When this shortening involves the connective component of the muscle, it generates a dual mechanical consequence:
- Resistant Force (RF): resistance to elongation that maintains constant traction on bone insertions, influencing joint alignment
- Working Force (WF): actual capacity to generate useful movement, reduced when part of the energy is absorbed by the internal resistances of the shortened tissue
Vector analysis allows prediction of which joint alterations will emerge when anatomically dominant muscles increase their RF, and identification of which muscular vectors maintain the observed alteration.
These principles are introduced here to provide a conceptual framework. Their physical basis and full clinical implications are developed in detail in the subsequent sections (from “The Biomechanical Framework: Core Principles” onward) and in the theoretical e-book.
The clinical observations documented by Françoise Mézières from 1947 onward represent the origin of this biomechanical approach.
The work developed within AIFIMM did not aim to create a new therapeutic technique, but to provide a coherent scientific framework capable of explaining, predicting, and verifying the mechanical effects observed in clinical practice.
To this end, the theoretical model was reformulated using principles of applied physics, while the therapeutic application remains the Mézières technique, preserved for its mechanical coherence and long-term clinical consistency.
Over more than four decades of clinical practice, this technique—compared with multiple manual approaches—has demonstrated stable results when systemic rebalancing is achieved, in agreement with biomechanical principles.
The interpretative model
This model is grounded in applied physics as it relates to the musculoskeletal system. Vector analysis of muscular forces, RF–WF mechanics, and anatomical dominances form the core clinical reasoning tools used to interpret dysfunction through demonstrable mechanical laws.
Joint misalignments are not treated as random events or “postural anomalies,” but as predictable outcomes of force resultants generated by structural shortenings and anatomical dominances.
Because of this, the model is transferable: it can guide clinical reasoning independently of the therapeutic tool used, provided mechanical coherence is respected.
The clinical practice
In practice, the model is applied through the Mézières technique, selected for its mechanical coherence with these principles
This technique acts directly on connective tissue shortening and produces measurable effects on joint alignment. When systemic rebalancing is achieved, clinical results tend to remain stable over time.
By its nature, the Mézières technique is non-protocolizable. It requires continuous adaptation based on patient response and on the mechanical effects observed during assessment and intervention.
Clinical application is therefore adaptive and individualized: intervention strategies evolve according to changes in tissue behavior, joint positioning, and global system response, rather than following predefined sequences.
The clinical application is taught by clinicians trained directly with Françoise Mézières (Paris, 1988–1990), integrating explicit biomechanical criteria with a clinically testable reasoning process.
| INTERPRETATIVE MODEL | CLINICAL PRACTICE derived from the interpretative model |
|
|
The e-book presents the complete theoretical framework underlying the course, including:
-
Physical foundations
Why muscles shorten structurally and how this generates joint dysfunctions and mechanical conflict
(RF–WF mechanics, connective tissue behavior under sustained load) -
Vector-based biomechanical analysis
Predicting joint and axial alterations through anatomical dominances and force resultants at key regions -
Clinical reasoning framework
Distinguishing primary causes from compensatory adaptations · Local vs. referred pain · Differential diagnostic criteria -
From principles to therapeutic strategies
Translating physical laws into clinical decisions: isometric contractions in lengthening, sequencing of intervention, and criteria for effectiveness and long-term stability -
Systemic integration
The musculoskeletal system as a complex adaptive system and its implications for stability, recurrence, and long-term outcomes
[Download E-book (PDF)]
[Download Course Program (PDF)]
Both resources are freely accessible.
Official Evaluation — The CPD Certification Service (UK):
"An advanced online course providing rehabilitation professionals with a scientifically grounded model for assessing and treating musculoskeletal dysfunctions through systemic biomechanics.
Based on the principles of the Mézières Method, it integrates physics, myofascial chain analysis, and vector-based muscle assessment to identify primary and secondary shortenings, optimize joint alignment, and restore functional balance.
Includes 32h of video lessons and 6h of reading materials, with demonstrations, case studies, and diagnostic tools."
|
| Official Certifications and Institutional Accreditation |
Officially certified:
Additional institutional accreditation The Italian-language edition of this same course has been accredited with 50 ECM credits by the Italian Ministry of Health — the national mandatory continuing education system for healthcare professionals in Italy. |
| On-Demand Onile Course |
All content is pre-recorded and available 24/7 for 12 months. |
| Watch a Free 2-Hour Sample Lesson |
Watch a free 2-hour sample lesson Original Italian lectures, fully dubbed in English by professional voice actors. |
| Independent Validation & Adoption | Trusted by over 6,000 physiotherapists.
Official ECM evaluations (Italy, Ministry of Health 1997–2025):
|
| 38 hours of structured online training | 32h HD video + 6h guided readings, with manual and 25+ downloadable resources |
| For physiotherapists, osteopaths, and rehabilitation professionals | Designed for licensed clinicians seeking advanced tools in segmental and systemic MSK biomechanics |
| International recognition | CPD certification is recognized in many European countries, Australia, and New Zealand. In Canada and other Commonwealth countries, it is often recognized or accepted depending on local regulations |
Scientific Publications (CPD-Selected)
The CPD Certification Service has selected and published several articles on musculoskeletal biomechanics, reflecting the scientific framework underpinning this course:
- Muscle Shortening and Joint Dysfunction – Physical and Clinical Mechanisms
- Body Equilibrium – A Physical-Clinical Interpretation of Human Upright Stability
- Vector Analysis in Musculoskeletal Biomechanics - Part 1: Foundations and Clinical Principles
- Vector Analysis in Musculoskeletal Biomechanics - Part 2: Clinical Applications and Case Interpretation
- Vector Analysis of the Vertebral Column in the Sagittal Plane - Clinical Application to Vertebral Equilibrium
- The Hyoid Bone: Biomechenical Analysis of a Mechanical Convergence Point-Force Redistribution in the Cranio-Cervical District
These publications reflect the scientific background and methodological principles that underpin the course “Systemic and Segmental Musculoskeletal Biomechanics”.
| Course Instructors
Mauro Lastrico, PT & Laura Manni, PT Over 40 years of clinical experience | 6,000+ physiotherapists trained | Author of Musculoskeletal Biomechanics and the Mézières Method (3rd ed.) |
The Biomechanical Framework: Core Principles
This section introduces the theoretical foundations that structure the entire course.
These principles—taught progressively through 18 on-demand video modules—explain:
• why joints and spinal segments alter,
• how these alterations can be predicted,
• and when intervention is required at a local and/or systemic level.
Each principle is immediately connected to clinical application, with real patient demonstrations showing how abstract physical laws translate into precise therapeutic decisions.
Why Muscles Shorten: The Physical Basis
In clinical practice, a consistent phenomenon is observed: even in the absence of specific pathologies, muscles tend to progressively shorten over time, altering both static alignment and joint dynamics.
This phenomenon is interpreted through the physical laws of material deformation applied to muscle tissue.
The Physical Structure of Muscle
From a biomechanical perspective, muscle is not a homogeneous structure but consists of two components with distinct mechanical behaviors:
• Contractile component (actin–myosin): behaves as an elastic material. After contraction, it returns to its initial length.
• Connective component (the connective tissue surrounding and supporting muscle fibers): behaves as an elastoplastic material. When subjected to prolonged tension, it maintains residual deformation proportional to the product force × time.
This is not pathology—it is physics applied to biological tissues.
The Mechanical Consequences
When the connective component shortens structurally, it generates permanent tension that acts continuously on the skeleton. Because muscle acts exclusively through traction and the skeleton adapts passively to force resultants, muscular shortenings become a primary determinant of joint axis alterations.
On these physical foundations rests the RF–WF model, which represents the core of the biomechanical interpretation taught in this course.
A structurally shortened muscle generates two distinct forces with opposite mechanical effects:
Resistant Force (RF)
The resistance the shortened muscle opposes to elongation.
→ STATIC consequence: constant traction on bone insertions, progressive alteration of joint axes, and asymmetric load distribution on articular surfaces.
Working Force (WF)
The muscle’s actual capacity to generate useful movement.
→ DYNAMIC consequence: as RF increases, part of the energy produced during contraction is dissipated in overcoming internal connective resistance. Movement becomes energetically inefficient, compensatory patterns emerge, and mechanical efficiency decreases.
These two forces are inversely proportional:
an increase in Resistant Force necessarily produces a decrease in Working Force.
Clinical Example: Psoas Muscle and Lumbar Lordosis
When the psoas muscle shortens structurally—even by as little as 2% of its length:
• its connective component maintains constant traction on the lumbar vertebrae (L1–L4)
• this permanent traction (high RF) shifts the vertebral bodies anteriorly, increasing lumbar lordosis
• posterior disc compression increases
• simultaneously, the psoas’ capacity to generate efficient hip flexion (WF) decreases, because part of its contraction is absorbed by internal tissue resistance
The abdominal muscles, though active, cannot counteract this effect:
this is not a problem of “strength” or “weakness,” but of vector mechanics.
The Clinical Paradox
A shortened muscle is simultaneously:
• “too strong” from a static perspective (high RF that alters joint alignment)
• “too weak” from a dynamic perspective (reduced WF that compromises functional performance)
Resistant Force and Working Force are therefore inseparable:
an increase in one determines a decrease in the other.
On these physical foundations, the entire clinical reasoning of the model is built.
Clinical Application
When palpating a shortened muscle, the clinician is perceiving the coexistence of two mechanical problems:
tissue that blocks joint motion (high RF) while simultaneously failing to perform its work efficiently (low WF).
It is like driving with the handbrake engaged: more force is required to move, but that force does not translate into effective motion—it is dissipated internally.
For this reason, asking a patient to “strengthen” a shortened dominant muscle often worsens symptoms: power is added to the engine without releasing the brake.
Recognizing this distinction fundamentally changes both assessment and therapeutic strategy.
Once it is clear why muscles shorten, the model takes the next step:
explaining why joint alterations do not occur randomly, but follow recurrent and mechanically predictable directions.
This predictive capacity is made possible through vector analysis of muscular forces.
What Vector Analysis Means in Clinical Practice
Every muscle can be represented as a vector: a line of force defined by its magnitude (how much it pulls), its direction, and its point of application.
When multiple muscles act on the same joint, their forces combine according to the laws of vector physics, generating a resultant that determines the final position of the bone in space.
Vector analysis allows the clinician to anticipate this resultant—and therefore to predict the direction in which a joint will tend to deviate as Resistant Force increases.
Anatomical Dominances: Why Alterations Are Predictable
Muscles are not distributed symmetrically around joints.
Within every agonist–antagonist system, intrinsic anatomical asymmetries exist—in muscle number, cross-sectional area, line of force length, and direction of traction. These asymmetries create genuine vector dominances that are independent of training, posture, or voluntary motor control.
When Resistant Force increases, anatomically dominant vectors emerge first and drive the loss of physiological joint sequencing.
These are not “random compensations,” but the predictable outcome of physical laws applied to anatomy.
Example: Shoulder Joint and Internal Rotator Dominance
In the glenohumeral joint:
Internal rotators: subscapularis, pectoralis major, latissimus dorsi, teres major
External rotators: infraspinatus, teres minor
The dominance of internal rotators is determined by three anatomical factors:
• Number: four internal rotators versus two external rotators
• Cross-sectional area: significantly greater overall muscle mass
• Length and direction: force lines that collectively generate a greater vector resultant
When Resistant Force increases in these muscles:
• the humerus is maintained in permanent internal rotation (static alteration)
• the humeral head is pushed anteriorly (axial deviation)
• the subacromial space is reduced, creating mechanical conflict
The external rotators, though active, cannot compensate: their vector resultant is structurally inferior.
This is not muscle weakness—it is physics applied to anatomy.
Other Recurrent Patterns
By the same biomechanical logic:
• the scapulae tend toward adduction with reduction of physiological thoracic kyphosis (dominance of scapular adductors)
• the foot tends toward supination and cavus, often with proximal compensations (dominance of supinators)
• the pelvis tends toward anteversion (dominance of psoas and spinal extensors)
From Static Alignment to Movement
In clinical observation, these patterns are already present in static posture.
The humerus does not “internally rotate” during movement—it is already internally rotated before movement begins.
Like a crack in a wall that follows lines of least resistance, anatomical dominance is expressed at rest, and movement merely amplifies it. This is why assessment begins with observation: it already indicates where causal vectors are likely located.
A Paradigm Shift in Clinical Reasoning
Clinical reasoning changes fundamentally.
Instead of starting from observation and searching for an explanation, the clinician begins with knowledge of anatomical dominances to predict alterations, verify them during assessment, and rapidly identify the vectors responsible for dysfunction.
This predictive framework is also confirmed in neurological conditions: when central inhibitory control is lost, as in spastic hemiparesis, the same anatomical dominances emerge in amplified form. Different mechanisms, same structural reality.
Connection with the RF–WF Model
The link with the RF–WF model is direct.
When Resistant Force increases in anatomically dominant muscles, subdominant vectors can no longer compensate, and joints deviate along anatomically predictable directions.
On this basis, vector analysis becomes a precise clinical tool:
it orients assessment from the outset, reduces interpretative variability, and guides intervention toward causal vectors rather than symptoms.
The model integrates prediction and observation: knowing anatomical dominances allows clinicians to anticipate which alterations will emerge—and to verify them clinically.
In this model, muscle shortening is not considered a local or obscure event, but the final outcome of tone regulation processes involving multiple interacting systems.
Regardless of the initial trigger, muscle represents the final effector—the structure through which the body realizes adaptation. For this reason, the model distinguishes different levels of origin while maintaining a unified biomechanical interpretation.
Neurophysiological Level
Basal muscle tone is regulated by sensory–motor integration circuits.
The nervous system uses muscle tone as a protective strategy through both reactive and anticipatory mechanisms:
• reactive responses emerge after pain has appeared,
• anticipatory responses act preventively to reduce the risk of potential pain.
When these contractions are maintained over time, they progressively involve the connective component of muscle, transforming transient tone increases into structural shortenings. This process lies fully within the scope of physiotherapy, as it manifests in the musculoskeletal system and produces observable mechanical consequences.
Biomechanical Level
Increased muscle tone may also represent an adaptive response to altered mechanical conditions—changes in load distribution, joint axes, or centers of gravity.
The system preserves functional equilibrium at the cost of a self-reinforcing cycle:
mechanical alteration → increased tone → structural shortening → further mechanical alteration.
The result is increased Resistant Force, reduced Working Force, loss of mechanical efficiency, and progressive rigidity. This level also belongs to physiotherapy, as it produces joint alterations that can be assessed, predicted, and treated.
Psychosomatic Modulation
A further level described in the literature involves prolonged emotional or stress-related states that modulate muscle tone through neurovegetative and central mechanisms. Over time, these influences may contribute to stable musculoskeletal patterns and orthopedic presentations.
In the model, this level does not require a different biomechanical interpretation: regardless of origin, its effects converge on muscle tone and connective tissue behavior.
The Common Denominator
Whatever the level of origin, the common denominator remains the same:
the system ultimately expresses adaptation through muscle.
As a result, very different clinical histories may converge toward similar muscular shortenings and compensatory patterns.
Clinical Application
In practice, the shortened muscle often represents the “final stop” of very different adaptive pathways.
One patient with chronic low back pain may present structural shortenings originating from altered mechanical loading; another from long-standing protective pain strategies following trauma; another from distant compensations, such as an unresolved foot dysfunction that modified weight-bearing patterns.
Despite different origins, the final presentation—accentuated lumbar lordosis, anterior pelvic tilt, shortened psoas—may appear identical.
For this reason, assessment cannot stop at describing what is observed, but must determine which level actively maintains the shortening, in order to avoid treating only the final effect.
The Task of Clinical Reasoning
The task of the model is not to identify every possible cause, but to interpret what is biomechanically relevant:
to distinguish between primary causes, muscular adaptations, and articular consequences.
On this foundation, the analysis of the musculoskeletal system as a complex adaptive system is introduced.
The human musculoskeletal system is, in every sense, a complex system. This means that no region functions in isolation and that any local intervention inevitably produces adaptations at a systemic level.
Complex systems theory describes systems composed of many interdependent and interacting elements. In such systems, the site of the symptom does not necessarily coincide with the location of the primary mechanical problem.
Historically, the concept of muscle chains represented an initial step beyond purely segmental thinking. In this model, the behavior of muscle chains is interpreted through demonstrable physical laws, integrating anatomy, force vectors, and joint mechanics into a coherent systemic framework.
Clinical Consequences of Systemic Organization
In a complex system, local pain may represent the expression of an altered systemic organization. Attempts at isolated correction can therefore be not only ineffective, but mechanically counterproductive.
This explains why instructions such as “stand up straight” or voluntary self-corrections are often ineffective: they increase global muscle tone and Resistant Force, worsening the system’s overall energy balance.
Emergent Abilities and Compensatory Strategies
A defining characteristic of complex systems is the emergence of compensatory strategies.
When specific muscles become mechanically ineffective due to excessive shortening, the system does not fail. Instead, it bypasses them, activates alternative synergies, and develops substitution patterns.
This is clearly observable during movement. When a patient is asked to raise the arm, the scapula may move before the humerus; when a leg is lifted, the pelvis may shift to compensate. These patterns are not “incorrect”—they represent the only available strategy for completing the task when the primary muscles are unable to function effectively.
Like taking a winding detour when the main road is blocked, the system succeeds in completing the movement, but at the cost of higher energy expenditure and increased mechanical wear.
This explains why isolated strengthening of subdominant muscles often fails to resolve dysfunction and why certain monoarticular muscles are systematically excluded from movement.
Efficiency and System Rigidity
In this model, a system functions efficiently when it operates near the edge of chaos—a condition in which Working Force prevails over Resistant Force.
When Resistant Force increases, the system becomes progressively rigid. Energy expenditure rises, physiological joint sequencing is lost, and movement efficiency decreases.
An efficient system moves fluidly, with smooth transitions between segments and minimal visible effort. When Resistant Force dominates, movement becomes fragmented and effortful, with pauses and compensations. Patients often report difficulty performing simple tasks—not due to weakness, but because every gesture requires disproportionate energy.
It is like pushing a shopping cart with locked wheels: effort increases, progress decreases, and fatigue appears rapidly.
Why Systemic Analysis Is Essential
For these reasons, systemic analysis is not an optional theoretical addition. It is the necessary condition for coherent clinical reasoning, for distinguishing cause from effect, and for selecting therapeutic strategies that are both effective and stable over time.
On these foundations, the model progresses from mechanical analysis toward structured clinical reasoning.
From Symptom to the Distinction Between Local Dysfunction and Systemic Organization
In musculoskeletal conditions, pain always represents valid clinical information, but it does not automatically coincide with the cause of the problem.
In some cases, pain is genuinely local and reflects a primary dysfunction of the symptomatic region. In other cases, the painful joint represents the outcome of an adaptive organization involving multiple body regions.
For this reason, the model never assumes a priori that pain is “referred” or systemic. On the contrary, clinical reasoning is founded on the need to distinguish local pain from secondary pain, avoiding generic interpretations or unverifiable explanations.
Tone, Adaptation, and Structural Change
The muscle tone observed in clinical practice reflects neurophysiological and biomechanical regulation processes aimed at maintaining stability and continuity of movement.
When these adaptive strategies persist over time, they may involve the connective component of muscle, leading to structural shortening and progressive alteration of physiological joint sequencing.
Pain often emerges when the system’s adaptive margins are reduced and mechanical efficiency declines.
Clinical Reasoning
Within the model, clinical reasoning integrates:
• observation of static and dynamic patterns
• analysis of anatomical and vector dominances
• targeted differentiation tests
The objective is to determine whether the symptomatic region is the primary source of dysfunction or the site of expression of a broader adaptive organization.
This distinction is essential, because it directly determines therapeutic strategy.
Local vs. Referred Pain
When pain originates locally, intervention on the symptomatic region can be resolutive and stable over time.
When pain is secondary or referred, treating only the site of the symptom may produce temporary relief, but improvements tend not to persist.
Clinical Application
A useful analogy is a warning light on a car dashboard. The problem may lie in the sensor itself (a local issue), or the light may be signaling engine overheating (a systemic issue). In the first case, addressing the sensor resolves the problem. In the second, replacing the sensor does nothing if the engine continues to overheat.
Similarly, shoulder pain may temporarily improve with local treatment, but if the primary restriction originates from an altered pelvic or spinal organization, symptoms will recur until the causal mechanical constraint is addressed.
Differentiation tests are therefore fundamental—not to label pain as “referred,” but to avoid treating the symptom without modifying the forces that regenerate it.
Primary vs. Secondary Muscle Shortening
A further key element of clinical reasoning is distinguishing between primary and secondary muscle shortenings.
In primary shortenings, the muscular system is the origin of joint misalignment, and vector rebalancing can be effective and stable.
In secondary shortenings, muscle represents an adaptation to dysfunction originating from other systems, requiring multidisciplinary assessment to avoid recurrence.
This distinction explains why some clinical improvements persist while others do not—not because treatment “works or fails,” but because the forces responsible for joint alteration have, or have not, been correctly identified and modified.
Whether pain is local or referred is not decided a priori. What matters is the ability to distinguish between them through precise biomechanical analysis.
The following simplified case illustrates how clinical reasoning is applied within the model. Real clinical situations are often more complex and require multiplanar assessment and continuous adaptation, but the decision-making logic remains the same.
Clinical case
A patient presents with anterior shoulder pain and limited abduction. No recent trauma is reported.
Phase 1 – Prediction through vector analysis
Based on anatomical dominances, vector analysis predicts internal rotator dominance. When Resistant Force increases in these muscles, the humeral head tends to shift anteriorly, reducing the subacromial space.
Phase 2 – Verification during assessment
Physical examination confirms the predicted pattern:
• anteriorized humeral head
• static internal rotation of the humerus
• scapular adduction
Phase 3 – Decision sequence
Intervention priorities are defined by force analysis, not by predefined protocols:
• address the subscapularis first (dominant vector in anteriorization)
• verify scapular repositioning, as adductors may maintain residual tension
• assess cervical compensations, frequently associated with scapular rigidity
Each step is guided by mechanical reasoning and continuously adjusted according to observed responses.
Phase 4 – Immediate verification
At the end of the session, key questions guide verification:
• has the humeral head repositioned?
• has abduction improved?
• is the system more elastic, or have new rigidities emerged?
If the answer is yes, the causal vector has likely been correctly identified.
If not, reassessment is required: are there unrecognized compensations? Is the shortening primary or secondary?
This is the clinical reasoning taught in the course: not “what to do for the shoulder,” but how to analyze the forces altering the shoulder and adapt intervention based on system response.
In real clinical practice, every patient requires individual assessment, consideration of systemic compensations, and strategies that evolve continuously in response to mechanical feedback.
How the Model Guides Clinical Intervention
In this model, physical principles do not generate rigid protocols, but clinical orientation criteria.
The therapeutic objective is not to correct a form or normalize an appearance, but to modify the forces that maintain the system in a mechanically inefficient state—reducing Resistant Force (RF) and restoring genuinely available Working Force (WF).
Why Contractile and Connective Components Require Different Approaches
Muscle is not a homogeneous tissue. Its contractile and connective components respond to different stimuli and cannot be treated with the same strategies.
Spontaneous movement—even when functional—is insufficient to re-lengthen a structurally shortened system. It always respects pre-existing safety limits established by the nervous system.
The shortened connective tissue lies beyond those limits. Reaching it requires guided therapeutic work, where the therapist progressively brings the patient beyond habitual boundaries under controlled and safe conditions.
For this reason, techniques acting primarily on tone or mobility may influence the contractile component, but remain insufficient when residual shortening is maintained by the connective substrate.
Primary Therapeutic Strategy
This is why the model employs isometric contractions performed in maximum physiological or relative elongation, within a strategy continuously adapted to system response.
A typical session integrates assessment, treatment, and verification.
Assessment
-
Static and dynamic observation to identify dominant vectors
-
Palpatory and visual verification of joint and vertebral misalignments
-
Differentiation tests to distinguish primary from compensatory patterns
Treatment
-
Patient positioning to progressively lengthen target muscles
-
Guided isometric contractions synchronized with prolonged active expiration
-
Continuous monitoring of compensatory escapes and tissue response
Verification
-
Re-testing previously limited movements
-
Checking for reduced pain, improved ROM, and increased system elasticity
Sessions are always individual, active, and guided.
What “Maximum Elongation” Means
Maximum elongation refers to the point at which tissue resistance increases but remains within patient tolerance—never forcing into pain.
Isometric contraction at this threshold reduces RF while respecting neuroprotective limits. This is controlled progressive loading, not aggressive stretching.
Precision in positioning, vector reading, and real-time observation is therefore clinically decisive.
The Role of Strength Training
Strength training is not excluded and is not considered harmful. It simply does not represent the initial phase when dominant vectors are shortened.
A subdominant muscle cannot modify joint alignment while a dominant vector expresses higher RF. Strengthening under these conditions increases effort but not correction.
Once mechanical balance has been restored, strengthening:
-
becomes effective
-
consolidates correction
-
increases WF
-
improves functional capacity and resilience
The approach does not oppose Exercise Therapy—it creates the conditions for it to work.
The Necessary Sequence
Mechanical rebalancing first
-
reduction of RF
-
vector reorganization
-
restoration of physiological joint alignment
Strengthening second
-
stabilization
-
performance improvement
-
recurrence prevention
Strengthening before rebalancing often reinforces compensation. Strengthening after rebalancing consolidates function.
Criteria for Treatment Effectiveness
Improvement is not defined by visual symmetry, but by three simultaneous outcomes:
-
local improvement
-
global tension reduction
-
increased system adaptability
If even one is missing, results tend to be unstable.
Clinical verification therefore asks:
-
Has pain reduced?
-
Has movement become more fluid?
-
Has tension relocated or genuinely decreased?
Adaptive Clinical Strategy
For this reason, the model does not propose standardized sequences, but an adaptive clinical strategy.
Intervention priorities vary according to present dominances and system response, always avoiding global rigidity and addressing the true mechanical conflict.
This approach proves particularly effective in chronic, recurrent, or resistant cases—when symptoms reappear because the forces regenerating them have not been modified.
Treatment as Clinical Reasoning
Treatment is never mechanical execution. It is clinical reasoning in action.
Technique remains subordinate to interpretation, the symptom is information, and effectiveness is measured by result stability over time.
It is within this balance—between biomechanical rigor and the human dimension of the therapeutic relationship—that the training pathway is founded.
This course does not require prior knowledge of advanced physics, mathematics, or vector calculus.
Biomechanical principles are introduced progressively, starting from direct clinical observation and practical cases, and only then connected to the underlying physical laws that explain what is observed.
Participants typically come from standard physiotherapy and rehabilitation training backgrounds. Through guided reasoning, real clinical examples, and repeated verification in practice, they progressively acquire vector-based analysis tools and learn how to apply them within clinical decision-making.
The objective is not theoretical abstraction, but functional understanding: enabling clinicians to recognize patterns, predict mechanical consequences, and reason coherently, even when dealing with complex or non-standard presentations.
This model does not derive its complexity from manual skill execution.
The therapeutic techniques themselves are accessible, safe, and learnable by any licensed clinician. What makes the model demanding is not how to perform a technique, but how to reason clinically in order to decide what, when, and why to treat.
In other words, the technique is simple.
The challenge lies in the decision-making process that guides assessment and intervention.
What Makes the Model Clinically Demanding
Identifying dominant muscular vectors
Understanding which force lines influence joint alignment requires biomechanical interpretation, not simple visual inspection.
Distinguishing primary mechanical causes from secondary compensations
Symptoms may be local, referred, or part of a systemic adaptive organization. Identifying the mechanical origin is a high-level clinical skill.
Recognizing the systemic impact of minimal shortenings
Even small connective-tissue shortenings (1–2%) can alter joint geometry and load distribution. Detecting these effects requires reasoning, not advanced manual techniques.
Predicting axial deviations through vector analysis
The model is not protocol-based. It relies on the clinician’s ability to predict how muscular vectors influence joint axes, both locally and at a distance.
Choosing the correct entry point and treatment sequence
A local correction may either improve or destabilize the overall system. Knowing where to intervene first—and what to avoid—is decisive.
A Simple Technique, a Complex Model
Many clinicians completing the course report the same experience:
“The techniques are easy to learn. What is demanding is changing the way you think.”
The value of the model does not lie in manual execution, but in the ability to:
-
interpret the musculoskeletal system as a network of interacting vectors
-
understand the relationship between Resistant Force and Working Force
-
read symptoms through systemic biomechanics
-
plan treatment with both local precision and systemic coherence
In Summary
The model is simple to apply, but requires clinical maturity and advanced reasoning.
What is taught is not a set of techniques, but a framework for interpreting biomechanical complexity and guiding coherent clinical decisions.
“Understanding vectors means knowing where to intervene—and in what sequence.”
— Mauro Lastrico, PT
About the sections above:
The theoretical framework presented earlier allows you to evaluate the model before enrolling.
The modules below show how this theory is taught progressively through video demonstrations, with each concept immediately applied to real patient cases.
Here's how the 18 video modules are structured:
Visual Learning: From Vector Analysis to Clinical Application
Each module integrates theoretical vector analysis with practical clinical demonstrations.
The course uses detailed anatomical diagrams showing force lines, dominant vectors, and mechanical conflicts, alongside live demonstrations of how this analysis translates into precise patient positioning and treatment strategies.
This visual integration ensures that abstract biomechanical concepts become immediately applicable clinical tools.
-
Theoretical Foundations and Assessment (videos 1–4 – 8h 30min)
Causes of muscular shortening, concepts of Resistant Force and Working Force, vector analysis applied to the muscular system, biomechanical principles, effects of isometric contraction in maximum physiological or relative elongation of the muscle fiber as a therapeutic tool, three-dimensional visual and palpatory assessment of the patient, manual techniques, and modalities of active work performed by the patient. Theory and practical demonstrations.
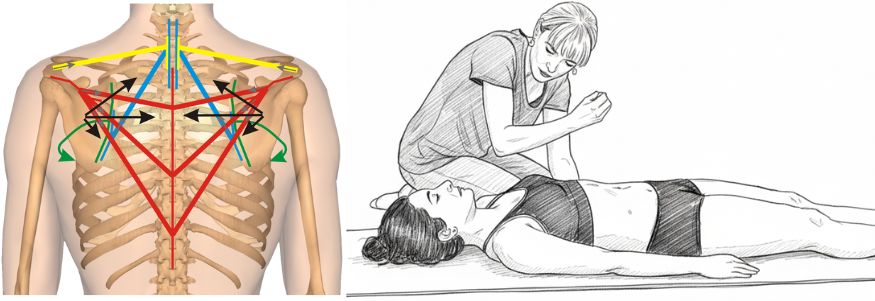
The core innovation: transforming anatomical muscles into force vectors to predict their mechanical effects. Left: Vector analysis reveals how shortened muscles create predictable force patterns affecting scapular positioning. Right: Clinical application where the therapist uses this vector understanding to guide treatment, working with therapeutic breathing to reduce resistant forces.
-
Sagittal Plane Corrections (videos 5–6 – 3h 55min)
Evaluation and corrective treatment, both segmental and systemic, of the cranio-vertebro-sacral system in the sagittal plane. Theory and practical demonstrations.
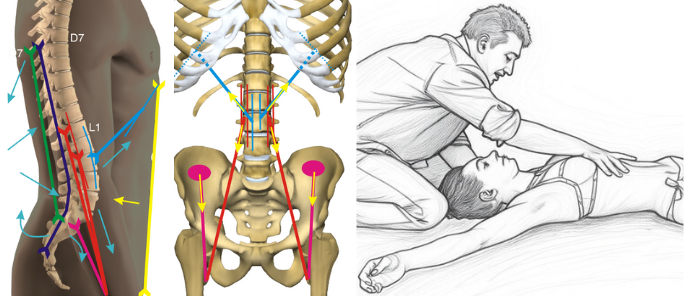
Vector analysis of forces acting between D7 and sacrum with their resultant force lines. Clinical application exemplifies how vector understanding guides therapeutic positioning - one example from the comprehensive toolkit of sagittal techniques presented in the course.
-
Frontal and Rotational Plane Corrections (videos 7–9 – 5h 51min)
Evaluation and corrective treatment, both segmental and systemic, of the cranio-vertebro-sacral system in the frontal plane; evaluation and treatment of upper limb pathologies and their connection with vertebral, costal, and hyoid dysfunctions. Theory and practical demonstrations.
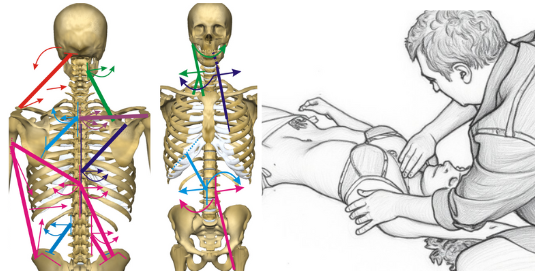
Vector analysis in the frontal plane reveals asymmetries and rotational patterns of the cranio-vertebro-pelvic system. Mechanical connections between upper limb and vertebro-costal complex guide integrated treatment - one of the specific approaches for frontal and rotational dysfunctions.
-
Lower Limbs and Specific Techniques (videos 10–12 – 5h 36min)
Evaluation and treatment, analytical and systemic, of lower limb pathologies and their relationship with vertebral dysfunctions. Theory and practical demonstrations.
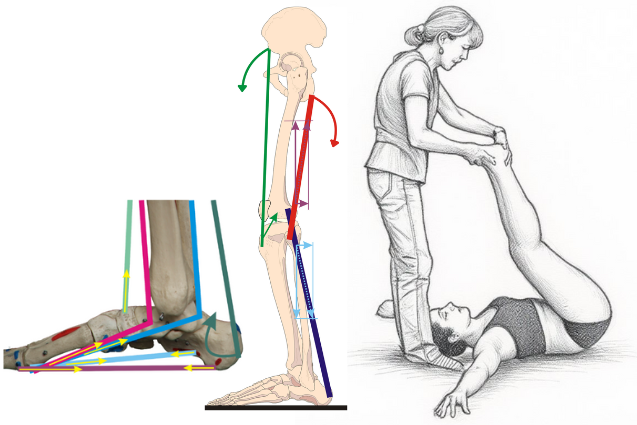
Vector representation of force lines acting on medial plantar arch and lower limb, with example of their treatment. These mechanical relationships enable both local and systemic therapeutic interventions.
-
Specific Districts (videos 13–15 – 5h)
Distinction between primary muscular problems and those secondary to structural alterations from other systems. Evaluation and treatment of TMJ disorders and the multidisciplinary approach, dynamic analysis and identification/treatment of altered patterns, treatment of humeral and sternoclavicular subluxations. Theory and practical demonstrations.
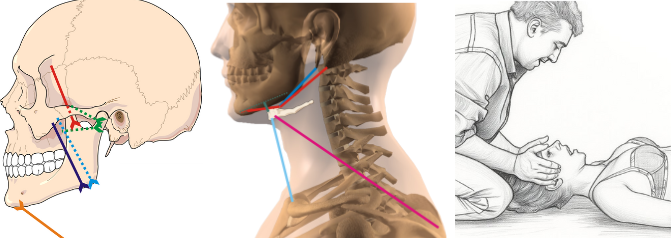
Vector analysis of temporomandibular joint, hyoid bone and cervical connections, with specific clinical application. Understanding these anatomical relationships determines whether direct treatment or multidisciplinary referral is indicated.
-
Clinical Reasoning (videos 16–18 – 3h 04min)
The symptom as an expression of a local or referred problem; from static and dynamic objective examination to treatment planning. Scoliosis: evaluation and treatment. Theory and practical demonstrations.
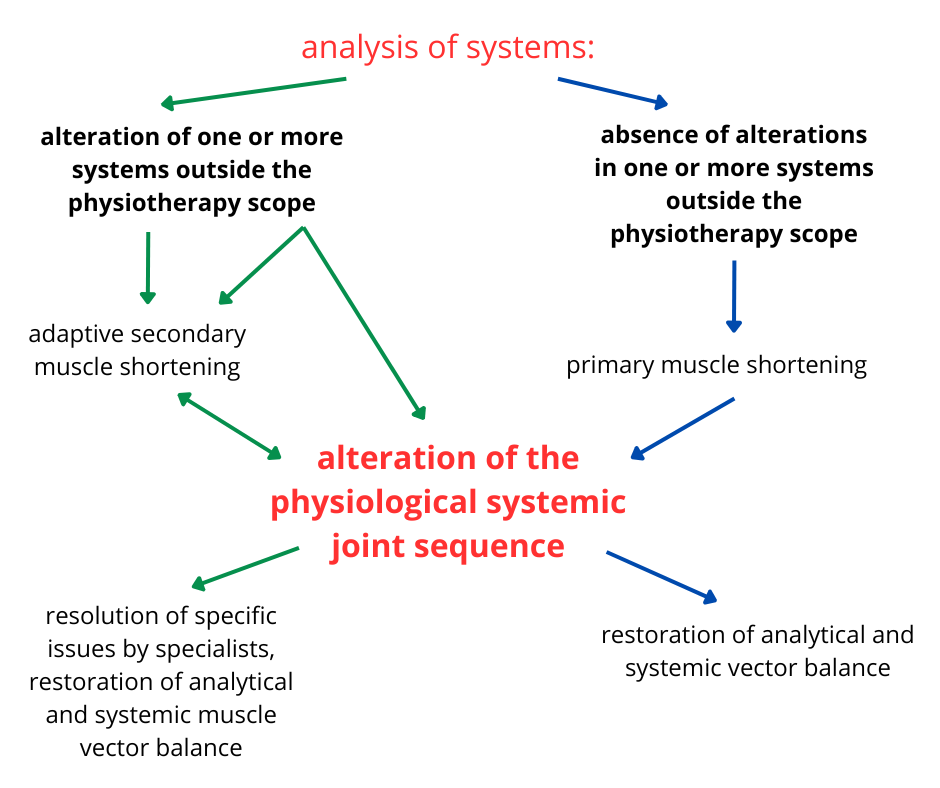
Systemic clinical reasoning: from systems analysis to treatment planning. The diagram illustrates the decision-making process for distinguishing between primary muscle shortenings (directly treatable) and secondary ones (requiring multidisciplinary approach), guiding optimal therapeutic strategy.
📌 Each video includes theoretical lessons, live demonstrations, and downloadable PDF materials. Download full program
The Institute
AIFIMM (Italian Association of Mézières Physiotherapists – Institute of Musculoskeletal Biomechanics) has been active since 1996, providing postgraduate clinical education in musculoskeletal biomechanics.
-
Officially accredited: ECM (Italy), CPD (UK), CEU (USA)
-
27+ years of continuous postgraduate education
-
Over 300 courses delivered
-
More than 6,000 physiotherapists trained
The Instructors
Mauro Lastrico, PT & Laura Manni, PT
Trained directly with Françoise Mézières (Paris, 1988–1990)
Mauro Lastrico and Laura Manni have over 40 years of clinical experience in musculoskeletal rehabilitation. Their training in Paris occurred during the final phase of Françoise Mézières’ teaching activity, at a time when empirical clinical practice was progressively being formalized into structured clinical reasoning.
Over the past three decades, they have systematized these clinical foundations into the physics-based biomechanical model taught in this course, integrating vector analysis, connective tissue mechanics, and joint axis sequencing.
Together, they have taught postgraduate courses to more than 6,000 physiotherapists and contributed to the development of the AIFIMM systemic assessment and treatment framework.
Mauro Lastrico is the author of Musculoskeletal Biomechanics and the Mézières Method (3rd ed., 2023).
Teaching Quality — Official ECM Data
(Italian Ministry of Health, 1997–2024 — 6,147 evaluations)
-
78% rated the training very useful, 21% useful
-
71% rated overall educational quality excellent, 27% very good
-
75% rated theoretical content delivery excellent
-
77% rated practical content delivery excellent
-
Over 90% would recommend the course to a colleague
(Official ECM data — Italian Ministry of Health)
Structured Online Training
✓ 18 video modules (32 hours) + 6 hours of guided readings and downloadable materials
✓ On-demand access: available 24/7 for 12 months
✓ Live demonstrations with detailed biomechanical analysis on real patients
✓ Dedicated chat support with Mauro Lastrico and Laura Manni throughout your learning journey
✓ Complete textbook and all supplementary materials in English (PDF)
✓ Over 25 downloadable clinical resources
Instructors are available for clarifications, clinical doubts, and in-depth discussions throughout the entire course.
Online Learning and Practical Application
The online course provides theoretical foundations, systematic progression through the biomechanical model, and live demonstrations with detailed vector analysis on real patients.
How technical precision is learned online:
Video demonstrations include:
- Precise anatomical landmarks for positioning
- Patient response indicators (breathing pattern changes, muscle tension variations, joint axis repositioning)
- Verification criteria to assess positioning accuracy
- Common errors and how to correct them
Palpatory assessment and positioning require direct practice, which should be organized independently or through supplementary in-person training. However, the course provides the visual and conceptual tools to self-correct and verify technical accuracy through objective patient responses: changes in joint alignment, variations in muscle tension, and patient feedback on perceived tension reduction.
Course fee
- One-time payment: €610
- Or 2 installments of €305
- Secure payments via Stripe (credit/debit card)
- No hidden fees, no renewals
Access
- Immediate after payment
- 12 months unlimited access
- HD streaming + complete PDF manual
Certification
- Digital certificate issued after course completion
- Granted upon passing the final test (20 multiple-choice questions)
- Delivered by email in PDF format at no extra cost
- Valid for:
- 38 CPD hours (UK) – The CPD Certification Service (Provider No. 21418)
- 45 contact hours / 4.5 CEU (USA, Florida) – CE Broker Provider ID 50-54885
Approved for 45 contact hours (4.5 CEU) — General Hours, PT & PTA.
CE Broker Tracking 20-1318645 · FPTA Approval CE25-1318645 · Effective 01/01/2026 – 12/31/2026.
FPTA disclaimer: "Accreditation of this course does not necessarily imply the FPTA supports the views of the presenter or the sponsors."
Available Research Evidence
The clinical application of the Mézières technique has received scientific validation through studies conducted in European university centers and published in peer-reviewed international databases.
Study Methodology:
- Design: Randomized controlled trials (RCTs)
- Primary outcomes: VAS, Roland-Morris, Berg Balance Scale
- Intervention duration: 5-24 weeks
- Results: Statistically significant efficacy superior to standard treatments (p<0.001)
These studies demonstrate superior efficacy compared to conventional treatments for chronic low back pain, postural alterations, and resistant musculoskeletal dysfunctions.
Why Research Is Limited (And Why This Isn't a Problem)
The Mézières technique has a distinctive characteristic that limits large-scale research: it is not protocolizable.
Each treatment requires:
- Individual biomechanical assessment
- Continuous strategy adaptation based on patient response
- Extended individual sessions (60 minutes)
- Therapists with advanced specific training
This individualization is the core of clinical efficacy, but makes the standardization necessary for large-scale RCTs impossible—which require rigid protocols replicable by different operators.
The AIFIMM Model: Biomechanical Rigor and Clinical Coherence
The theoretical framework developed by AIFiMM is founded on two complementary pillars:
1. Mechanistically-Reasoned Medicine
Clinical reasoning based on:
- Vector mechanics of the muscular system
- Elastic behavior of contractile and connective components
- Demonstrable relationships between shortening, RF-WF, and articular conflicts
- Complex systems physiology
- Coherence between acting forces and observable axial modifications
2. Evidence-Informed Practice
Critical use of available evidence, integrated with:
- Verifiable clinical observation
- Measurable outcomes over time
- Coherence between acting forces and observed axial changes
Every intervention is evaluated not only on immediate efficacy, but on stability over time.
This approach recognizes that a method's effectiveness depends not only on the number of published RCTs, but on coherence among physical principles, biological mechanisms, and observable clinical results.
Clinical Effectiveness: AIFIMM Data
Official ECM evaluations (5,000+ assessment forms, Italian Ministry of Health):
- Clinical relevance: 73% excellent
- Training usefulness: 78% very useful
- Practical teaching: 77% excellent
AIFiMM articles published by The CPD Certification Service (UK):
- Muscle Shortening and Joint Dysfunction – Physical and Clinical Mechanisms
- Body Equilibrium – A Physical-Clinical Interpretation of Human Upright Stability
- Vector Analysis in Musculoskeletal Biomechanics - Part 1 & 2
CPD UK certification obtained after independent content evaluation by international commission.
In Summary
The AIFIMM biomechanical model:
- Is based on a clinical technique (Mézières) with limited scientific evidence for structural reasons, not lack of efficacy
- Bases clinical reasoning on verifiable physical principles
- Produces stable results over time, documented by over 75 years of Mézières Method clinical practice
- Does not compete with protocolizable methods—it positions where personalization is necessary
The absence of large RCTs does not derive from methodological weakness, but from the impossibility of standardizing what is, by nature, individualized.
1. Is the course delivered in Italian?
No. All video lectures are original Italian recordings fully dubbed in English by professional voice actors. All written materials, textbooks, and resources are provided in English. The 2-hour free sample lesson demonstrates the English audio quality.
2. Are CPD/CEU credits recognized in my country?
- UK: Yes, 38 CPD hours fully recognized
- USA (Florida): Yes, 45 contact hours / 4.5 CEU officially approved
- EU, Australia, New Zealand: CPD is widely recognized
- Canada: Often recognized, check with your provincial regulatory body
- Other countries: CPD certification from UK providers is generally accepted for continuing education portfolios
3. How much time per week do I need to commit?
The course is entirely self-paced with 24/7 on-demand access for 12 months. Most participants complete it in 3-6 months, dedicating 2-4 hours per week. You can adjust the pace based on your schedule.
4. What if I need more than 12 months to complete the course?
Access is guaranteed for 12 months from enrollment. If you need additional time, contact us before expiration—extensions can be arranged.
5. Do I need advanced physics or mathematics knowledge?
No. Biomechanical principles are introduced gradually using clinical examples. The focus is on practical application, not mathematical formulas. If you understand basic anatomy and physiology, you have the foundation needed.
6. Is there instructor support during the course?
Yes. All enrolled participants have access to a dedicated course chat (similar to a group discussion platform) where you can interact with both instructors—Mauro Lastrico and Laura Manni—and fellow course participants.
Instructors monitor the chat regularly and respond to clinical questions typically within 24-48 hours. Complex case discussions may receive more detailed responses. The collaborative format also means fellow participants often contribute insights from their own clinical experience.
This collaborative environment allows for clarifications, clinical discussions, case sharing, and in-depth exchanges throughout your 12-month access period.
7. Can I download the videos for offline viewing?
Videos are streamed on-demand (not downloadable) but available 24/7 for 12 months. All PDF materials, textbooks, and resources are downloadable. A stable internet connection is required for video streaming.